1. About the mental health and wellbeing JSNA toolkit
Updated 25 October 2019
1. Introduction
This toolkit signals the National Mental Health Intelligence Network’s (NMHIN) intent to support the development of mental health and wellbeing joint strategic needs assessments (JSNAs). It has been developed for those seeking to understand the breadth and complexity of mental health issues in their area, such as JSNA and mental health leads in local authorities and clinical commissioning groups (CCGs). It helps people to consider factors that affect mental health and wellbeing and to identify some of the key data, information and knowledge that local areas may use to build a picture of need.
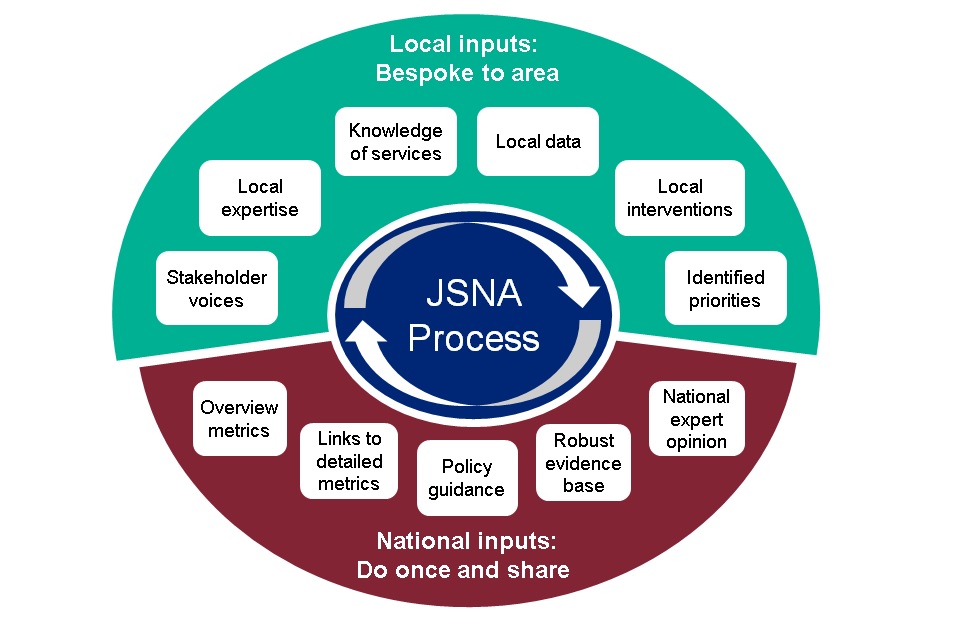
We have developed the toolkit to work as part of a national/local collaboration (figure 1) which:
Supports
Local areas hold the expertise and the responsibility for developing JSNAs. These resources will help reduce workload by doing centrally what can be done centrally and providing access to nationally available advice.
Respects variation
A ‘one size’ JSNA does not fit all. This toolkit is designed to be flexible enough to fit with and assist the locally derived process.
Figure 1: Collaboration model for JSNA development
1.1 Why develop a Mental Health and Wellbeing JSNA toolkit?
There are 2 reasons for the NMHIN to develop a toolkit.
Responding to local voices
With regards to JSNAs, national teams have been asked by local areas to take a lead and ‘do centrally what can be done centrally’ and share. More generally, local areas have asked the NMHIN to present metrics related to mental health at a lower geography and to provide explicit links between data and related policy and evidence. This toolkit is part of the effort to meet those requests.
The policy imperative
Recommendation 2 from the Five Year Forward View For Mental Health[footnote 1] directed Public Health England (PHE) to develop a national Prevention Concordat programme, within this was the action to support all health and wellbeing boards (along with CCGs) to put in place updated JSNAs and joint prevention plans. The NHS Long Term Plan makes a renewed commitment to improve and widen access to care for children and adults needing mental health support and opportunity to not only treat people, but also prevent them from getting ill in the first place. PHE’s new five year strategy includes an upgraded approach to mental health with a significant focus on prevention. This toolkit is part of the action to deliver these policy and strategic commitments. It continues to fit within the PHE Prevention Concordat for Better Mental Health work programme.
1.2 What is in the toolkit?
The structure and content of the toolkit is shown in figure 2. It illustrates what the national level role in the development of a local JSNA can be. That is to gather information and knowledge into one place to inform a local intelligence based approach to assessment of need.
The components of the toolkit are designed to work together to meet a range of needs. They provide an overview of the mental health care pathway and provide a gateway to detailed information and knowledge on particular aspects of mental wellbeing, mental illness prevention, and the care and support available for and required by those with a mental health problem.
Figure 2: JSNA toolkit structure: information + knowledge = intelligence
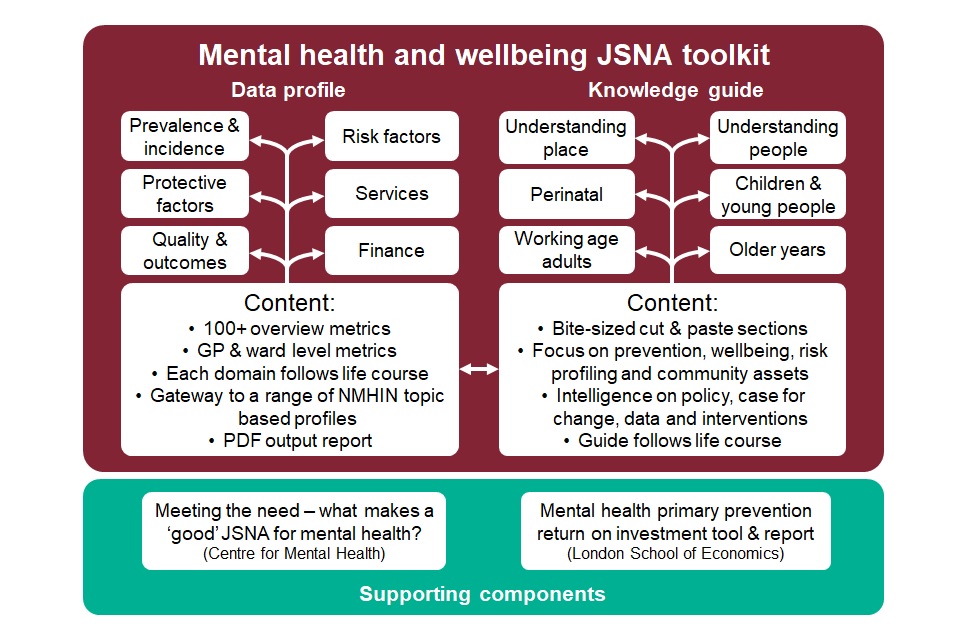
The toolkit has 2 main products:
MHW JSNA profile
Hosted on Fingertips, it includes around 100 metrics at various geographies that together provide broad coverage of the life course mental health pathway. It enables profiling of a local area and benchmarking of that area to meaningful comparison groups. It is a start point for considering topic related data and a gateway to further Fingertips hosted profiles.
MHW knowledge guide
Presents distinct short sections that should map well to most JSNA structures. It includes topic based links to the data profile and additional sources of data, and advice on data items to consider collecting locally. It includes links to topic-specific evidence on the case for change and recommended interventions, alongside links to policy.
The profile and guide link to and draw upon three other pieces of work. They are described as ‘supporting’ because they contribute to the Mental Health and Wellbeing JSNA process – each is also stand-alone and important. They are:
Meeting the need: what makes a ‘good’ JSNA for mental health?
This report funded by PHE and produced by The Centre for Mental Health, analyses how five councils across England developed their JSNAs to achieve real changes in their communities. It identified eight key success factors and provides advice and examples from five areas. It provides key messages to both national agencies and local authorities. The content and approach of this JSNA toolkit has been directly informed by the recommendations of this report
The ‘Promotion of mental health and wellbeing and prevention of mental disorders’ toolkit and report
The ambition of this work is to enable local areas to derive a mental health prevention programme appropriate to their population and to quantify the benefits of putting interventions in place. The topics covered within this report inform and are referred to at the appropriate places throughout the Knowledge Guide.
1.3 Prevention Concordat for Better Mental Health
The Mental Health and Wellbeing JSNA Toolkit is part of the wider PHE led Prevention Concordat for Better Mental Health. This programme of work promotes a more prevention focussed approach towards improving the public’s mental health. It aims to galvanise local and national action around the prevention of mental illness and promotion of good mental health by publishing a suite of resources designed to help every local area to put in place effective prevention planning arrangements.
1.4 Toolkit development
This toolkit provides guidance and attempts to map a relatively straightforward route through a complex and multi-faceted subject. Although this is an already useful resource the toolkit will be tested and developed over time. Feedback on its value is welcome and can be provided at [email protected].
It is also important to stress that the toolkit does not aim to replace other guidance materials, rather to link to and fit with them. It is not an attempt to provide the definitive resource or comprehensive coverage of all facets of mental health, rather to make available some direction and assistance on most topics related to mental health and wellbeing likely to form part of a JSNA.
2. Introducing the data profile
The mental health and wellbeing JSNA data profile fits with and works alongside the ‘Knowledge Guide’. It presents selected nationally available metrics that provide an overview of mental health and wellbeing in a way that is easily navigated.
Data are presented in 5 domains, broadly based on the pathway of progression of mental health conditions. These are:
- prevalence and incidence
- risk factors
- protective factors
- services
- quality and outcomes
Within each domain there is a clear substructure: first it follows life course, that is children, then adults, then older people, and within that it travels from universal to specialist, for example within ‘quality and outcomes’ in the CCG view, it considers primary care, then IAPT, then specialist mental health services.
Content
Data are drawn from many sources and vary by time period, population and presentation of values. Care should be taken with interpretation. Detailed metadata and any caveats are set out in the Definitions section of the profile.
Approach
The profile aims to provide enough whole-pathway metrics to enable local areas to assess current mental health need, services and outcomes. This can be a start point to identifying topics that require further investigation. Some areas will not wish to consider overview metrics and can use this toolkit to go directly to more detailed topic specific support.
Presenting geographies
The majority of metrics in this (and other Fingertips profiles) are presented by CCG or local authority. However, for the first time in a NMHIN profile, a small number of metrics are included by electoral ward and General Practice to provide an assessment of variation within the patch; where possible metrics are also presented by STP footprint.
Using the profile
The profile is hosted on Fingertips, the platform used to present NMHIN’s suite of profiles about mental health. Metrics can be presented in a number of ways and although, overall, it is relatively straight forward to use there are materials provided to help. The following resources are available:
- fingertips user guide Mental Health and Wellbeing JSNA: helps navigate the JSNA profile
- indicator list Mental Health and Wellbeing JSNA: profile content at a glance
Profile outputs
The data content of the profile is made available for use outside of Fingertips in a number of ways:
- exporting figures: all figures can be exported for use within local documents
- downloading data: all data can be downloaded in an excel file and used outside of Fingertips
2.1 Mental health profiles hosted by NMHDNIN on Fingertips
Rather than use the overview metrics provided in the JSNA data profile, some areas may wish to focus on topic specific detail. To facilitate this, below are links to key related profiles maintained by Public Health England.
- Children’s and Young People’s Mental Health and Wellbeing
- Common Mental Health Disorders
- Crisis Care
- Severe Mental Illness
- Co-occurring Substance Misuse and Mental Health Issues
- Perinatal Mental Health
- Suicide Prevention
- Dementia
2.2 Other related profiles hosted on Fingertips
There are additional topic specific profiles not maintained by the MHDNIN; These include:
- National Child and Maternal Health Intelligence Network (CHiMat)
- Local Tobacco Control Profiles for England
- Local Alcohol Profiles for England
- Productive Healthy Ageing
- Wider Determinants of Health
2.3 Changes to the profile
The aim is to report robust and stable metrics to support; assessment of local need, meaningful comparison, and assessment of change over time. For the most part profile content will stay constant enough to do this, but we must recognise we are in a time of significant change in data relating to mental health and wellbeing. Although this is good - more and better data will become available.
3. Introducing the MHW JSNA knowledge guide
This document fits with and works alongside the ‘MHW profile.’ It provides links to policy, guidance and evidence relating to understanding and meeting mental health need. It also provides access to:
- data contained within the data profile
- the wider suite of ‘Fingertips’ profiles
- additional data sets related to mental health and wellbeing
- suggestions around what relevant data can be collected locally
Structure
The guide begins with a focus on understanding the local population and in particular risk, wellbeing, prevention and community resilience. These are covered in the Mental health: environmental factors and Mental health: population factors documents. After that, the guide focusses on the care pathway, following a life course approach that includes documents on perinatal mental health, children and young people, working age adults and older people. Each of these documents begins with an introduction and a list of questions a JSNA may attempt to answer.
Then within each document there are a series of short topic based chapters that follow this standard format:
- overview
- data sources (national metrics and potential for locally collected data)
- evidence and further information (guidance and evidence on support and interventions)
Topics that do not have associated metrics in the data profile are covered but these are brief and direct the user to key external knowledge sources.
The evidence and further information sections are not exhaustive. The selection of links to source material has been made on the basis of outputs being relevant and produced by NICE, PHE or NHSE, or recommendation of consulted topic experts.
Approach
The guide aims to be clear and concise. Sections are short, in bite-sized chunks that are easy to navigate, and some text is designed to be cut and pasted. The document structure aims to assist the development of a complete picture of mental health needs. It is intended to help those seeking to cover all elements of mental health and it is not intended to be prescriptive.
Like the Data Profile, the guide is designed to provide both an overview and a route into a more detailed investigation. People who have already identified a small number of priority areas will be able to go directly to the relevant information.
What is missing
The knowledge guide aims to cover the main topics related to mental health likely to be included in local JSNAs. However, it does not seek to cover every related topic or to cover all topics in detail. There will be gaps and omissions and there are sections where detail is lacking. We will continue to consult on and improve the knowledge guide.
4. Key sources of information
Throughout the guide, supporting references are provided. However, the following sources have been drawn upon multiple times and we wanted to acknowledge their contribution and also identify them as particularly useful resources that aid development of a mental health and wellbeing JSNAs:
The Five Year Forward View for Mental Health outlines a new five-year national strategy for mental health in England. Created by the Mental Health Taskforce and commissioned by NHS England.
Better Mental Health for All by the Faculty of Public Health and the Mental Health Foundation summarises the evidence and outlines approaches and interventions for improvement.
Fundamental Facts about Mental Health by the Mental Health Foundationsummarises mental health research.
Chief Medical Officer (CMO) annual report: public mental health makes evidence based recommendations to improve public mental health services.
Future in Mind has recommendations to improve child and young people’s mental health from a taskforce co-chaired by NHS England and the Department of Health.
NICE resources for mental health and wellbeing outlines relevant quality standards and pathways’
Adult Psychiatric Morbidity Survey (APMS) provides data on the prevalence of both treated and untreated psychiatric disorder in the English adult population.
5. Endorsements and acknowledgments
5.1 Tim Kendall and Geraldine Strathdee
Professor Tim Kendall, National Clinical Director for Mental Health NHS England and NHS Improvement:
This JSNA toolkit will be a valuable resource to support local areas in their efforts to understand and improve mental health and wellbeing.The past 18 months has seen good progress in embarking on the transformation required to meet the ambitions set out in the Five Year Forward View for Mental Health, but there is still many opportunities for us to improve.
This toolkit will be essential for those involved in designing and developing services across the country to better ensure these meet the needs of their population.
This work would not have been possible without the stewardship and dedicated expertise of my predecessor, Geraldine Strathdee. Her contribution to advances in intelligence in mental health, including during her time as National Clinical Director, are well known, and I would like to pay tribute to her.
Geraldine Strathdee C.B.E. O.B.E. MRCPsych. Clinical Lead, National Mental Health Intelligence Network:
In England and globally, policy makers, scientists, and citizens are developing a growing awareness of the need for a new model for mental health. There is unprecedented interest and commitment to promoting mental health and wellbeing in people of all ages, building resilience in our populations and providing effective care to people that develop mental ill health. This welcome commitment comes from across the political spectrum and is a priority in local communities, front line public services, citizens’ advocacy bodies, and the media.
Within national and local government there is an understanding that public services need to help individuals and communities to make best use of their resources to focus on prevention and demand management. The greatest opportunities arise in the way we support children and their parents: 50% of all mental ill health starts before the age of 14 years, and 75% by 24 years.
Mental health as a speciality has led the way in innovation; from an hospital based model three decades ago, 89% of all mental health care now takes place in communities and home settings. Community partnerships are at the heart of good mental health care and collaboration between agencies to deliver needs led, biopsychosocial care is well understood. The ending of the strange dichotomy within health and care settings of focussing on people’s physical bodies separately from the emotions, behaviours and minds of their owners presents an opportunity to provide care and support in ways that make a real difference. Digital innovation brings new ways of identifying the avoidable causes of ill health and transforming access to information and treatments.
The aim of this JSNA toolkit is to provide knowledge to those who want to know more about mental health and how to use population health informatics and intelligence. It brings together the available top-level knowledge to support local planners and decision makers. It takes a life course approach, providing evidence of where individuals and communities can be supported to develop their own health and wellbeing, to maximise the use of self-management and peer and community assets. Throughout it has a focus on empowering people, communities and local partners to have the information and support they need to have the control and life chances that enable them to function at their highest level, bringing personal, social and economic capital to their lives and communities.
Throughout it has a focus on empowering local partners to have the information and support they need to understand mental health and wellbeing within their population and give due consideration to building resilience, promoting good mental health and wellbeing, and focusing on the preventive interventions that can make a real difference.
5.2 Jim McManus and Andrew Furber
Prof. Jim McManus, OCDS, BD(Hons), CPsychol, CSci, AFBPsS, FFPH, FCIEH, FRSB. Director of Public Health, Hertfordshire County Council:
If I could ask for one thing of national bodies it would be to understand where and how you can add value to local work. This toolkit makes a good contribution towards doing that.
The acid test of a tool or a resource for me at local level is this: can I stand up in front of elected councillors, local carers and service users and say this adds value to how we address an issue in our area? Will it help us improve the mental health of our residents? I’m very pleased to say this will.
I know that there are times when the word ‘toolkit’ makes people’s hearts sink as they anticipate a further compendium of stuff nobody really wanted and nobody can ever be found to have asked for. This is the second mental health tool in recent times I have come across which is very definitely not in that vein. The first was a tool for faith communities produced by liveability. The second is this. Both are practical, usable and could lead to tangible benefit to peoples’ health. For those reasons I am delighted to support and endorse this tool.
It doesn’t direct, it offers resources for people to use with local discernment. Most of us know that effective JSNA development and its translation into commissioning must be locally led, and is at its best when it comes out of good local relationships and partnerships. The tools in here have been developed with the involvement of people who lead and deliver JSNA programmes, so they know what can work and what won’t. To include that experience and nous in this process will, I think, be an essential ingredient in it working.
Similarly, national agencies make their best contribution to something like this when they bring to the table things others don’t have. And so this resource makes robust national level metrics available to all, enabling ward level variation to be measured and compared. That’s a vital contribution. It also makes suggestions about what data can be collected locally – suggestions which have been arrived at using local and national expertise working together.
And finally, this tool ensures that all of this data links to evidence about effectiveness. So this tool helps you go from data to benchmark to what works. That should make it easier for us at local level to identify need and plan for action to improve the mental health of our populations.
Dr Andrew Furber (GMC registration 3406915). Director of Public Health, Wakefield Council:
The approach of this toolkit is both practical and aspirational. We know that having a sound understanding of our local population mental health and wellbeing is vital to planning effective health and care services. This toolkit helps us get there, and does so in a flexible way – because not all areas require the same input.
I like the content of this toolkit. It covers a complex topic in a relatively straight-forward way. There are many sections, but they are brief and well-structured, and navigation is easy. I also like that PHE have produced an output that doesn’t only look at mental illness, it helps local areas give due consideration to building resilience, promoting good mental health and wellbeing, and focusing on prevention.
Lastly, I like a toolkit that acknowledges that it needs to improve – this is version 1, it’s good and worth using, but it will get better. I encourage all areas to use this toolkit, and to provide feedback on it, so that together we can aspire to make JSNAs that cover mental health and the actions that follow get better every year.
5.3 Authors
The toolkit has been produced and authored by the National Mental Health Intelligence Network with particular input from Sam Lane, Cam Lugton, Geraldine Strathdee, Kate Lachowycz, Rachel Roche, Gillian Bryant, Michael Streather, Simran Sandhu, Sue Foster, Arvinder Duggal, Alex Jones, Neil Hanchett, Danny Yip, Will Morris and Gabi Price.
These products, co-funded by NHS England, have been in development since 2016 and have benefitted hugely from the input of a wide range of colleagues from across the health sector. We are very thankful to those who have freely given up their time to support this important work.
5.4 Acknowledgements
We are particularly thankful for the contributions from:
Nuzhat Ali, Louis Appleby, Polly Ashmore, Andy Bell, Jo Black, Andrew Brown, Alistair Burns, Alison Burton, Qasim Chowdary, Emma Christie, David Conrad, Peter Cornish, Anne Cunningham, Majec Czachorowski, Janine Dellar, Felicity Dormon, Helen Duncan, Sarah Dunsdon, Rebecca Elleray, Robert Finnin, Andrew Furber, Helen Garnham, Rebecca Goldberg, Andrew Gordon, Allan Gregory, Xanthe Hannah, Maeve Hartwell, Corinne Harvey, Becky Hemming, Gregor Henderson, Sarah Holloway, Jeremy Hooper, Alyson Jones, Sarah, Khan, Tim Kendall, Julia Knight, Jane Leaman, Gill Leng, David Lyon, Lily Makurah, Sharon McAteer, Karen McCarthur, Coaimhe McKerr, Jim McManus, Mia Moilanen, Anne O’Herlihy, Andrew O’Shaughnessy, Clare Perkins, Bobby Pratap, Kathryn Pugh, Elaine Rashbrook, Jonathan Robertson, Claire Robson, Helen Shaw, Angela Snowling, Jez Stannard, Jude Stansfield, Sue Sylvester, Johanna Tipper, Briony Tatem, Hilary Tovey, Steve Taylor, Carly Tutty-Johnson, Elaine Varley, Stephanie Villanueva, Jo Wall and Stephen Yeung.
