Diphtheria: notifications, deaths and laboratory isolates data
Updated 1 June 2023
Applies to England and Wales
Summary of different measures
Notifications
Notifications are based on clinical reports of suspected cases of diphtheria reported by registered medical practitioners to the UK Health Security Agency (UKHSA) notifications of infectious diseases (NOIDs) system. Not all notified patients will have confirmed diphtheria nor will all confirmed cases be notified through NOIDs - with the disease considerably rare in the UK, clinical diagnosis may be missed and notifications are less accurate.
Local microbiology laboratories notify UKHSA via the Second-Generation Surveillance System (SGSS) on identification of a notifiable organism (see ‘Laboratory isolates’ below).
Deaths
Complications, including death, are attributable to the effects of the diphtheria toxin produced by Corynebacterium species. Without effective treatment, the toxin can spread through the blood to other organs causing functional damage, paralysis and death.
Laboratory isolates
Clinical laboratories that isolate C. diphtheriae, C. ulcerans or C. pseudotuberculosis locally send samples on to the national reference laboratory for toxigenicity testing. Not all Corynebacterium species are toxigenic (that is, produce the disease-causing toxin), therefore the number of isolates received at the reference lab will outweigh the final number of confirmed cases. Numbers of isolates reported may differ to number of cases in other reports which are based on year of onset of symptoms.
Case
A case is identified by isolation of diphtheria toxin-producing C. ulcerans or C. diphtheriae (indicated by PCR and later confirmed by Elek test) from a clinical specimen by a reference laboratory. Patients presenting with classic respiratory diphtheria[footnote 1] but that do not have laboratory confirmation of a toxigenic strain, can be classed as a confirmed case if they have an epidemiological link to a laboratory-confirmed case with a toxigenic strain. Patients that do not present with symptoms but do have laboratory confirmation of a toxigenic strain are classed as asymptomatic carriers of a toxigenic strain, and public health action for these carriers should be implemented as for confirmed cases.
Diphtheria notifications and deaths in England and Wales from 1986 onward
Notifications and deaths are based on data from ONS where diphtheria is listed as cause of death. Data may be incomplete for the current year.
Table 1. Diphtheria notifications and deaths in England and Wales, 1986 to 2022
From 2016 onwards, data is from England only.
| Year | Corrected notifications: total notifications | Corrected notifications: number due to toxigenic C. diphtheriae | Corrected notifications: number due to toxigenic C. ulcerans | Corrected notifications: number due to non-toxigenic Corynebacteria | Deaths |
|---|---|---|---|---|---|
| 1986 | 4 | 3 | 1 | 0 | 0 |
| 1987 | 2 | 2 | 0 | 0 | 0 |
| 1988 | 1 | 1 | 0 | 0 | 0 |
| 1989 | 2 | 1 | 0 | 1 | 0 |
| 1990 | 2 | 1 | 0 | 1 | 0 |
| 1991 | 2 | 1 | 0 | 1 | 0 |
| 1992 | 8 | 1 | 0 | 7 | 0 |
| 1993 | 6 | 5 | 0 | 1 | 0 |
| 1994 | 9 | 0 | 1 | 8 | 2 (see note 1) |
| 1995 | 12 | 1 | 0 | 11 | 0 |
| 1996 | 11 | 2 | 0 | 9 | 0 |
| 1997 | 22 | 2 | 0 | 20 | 0 |
| 1998 | 23 | 1 | 1 | 21 | 0 |
| 1999 | 23 | 0 | 0 | 23 | 0 |
| 2000 | 19 | 1 | 0 | 18 | 1 (see note 2) |
| 2001 | 13 | 0 | 1 | 12 | 0 |
| 2002 | 20 | 2 | 1 | 17 | 0 |
| 2003 | 13 | 0 | 0 | 13 | 0 |
| 2004 | 10 | 0 | 2 | 8 | 0 |
| 2005 | 9 | 0 | 1 | 8 | 0 |
| 2006 | 10 | 0 | 1 | 9 | 1 (see note 3) |
| 2007 | 9 | 0 | 0 | 9 | 0 |
| 2008 | 6 | 0 | 0 | 6 | 1 (see note 4) |
| 2009 | 11 | 0 | 2 | 9 | 0 |
| 2010 | 8 | 1 | 1 | 6 | 0 |
| 2011 | 2 | 0 | 0 | 2 | 1 (see note 5) |
| 2012 | 1 | 0 | 0 | 1 | 0 |
| 2013 | 9 (see note 6) |
2 | 0 | 5 | 0 |
| 2014 | 14 | 0 | 0 | 14 | 0 |
| 2015 | 9 (see note 7) |
1 | 2 | 4 | 0 |
| 2016 | 9 (see note 8) |
0 | 1 | 7 | 0 |
| 2017 | 13 | 0 | 0 | 13 | 0 |
| 2018 | 21 | 2 | 0 | 19 (see note 9) |
0 |
| 2019 | 8 | 0 | 0 | 8 | 1 (see note 2) |
| 2020 | 1 | 0 | 0 | 1 (see note 9) |
0 |
| 2021 | 3 | 1 | 0 | 1 (see note 9) |
2 (see note 2) |
| 2022 | 22 (see note 10) |
3 | 0 | 8 | 0 |
Note 1 - 1 death incorrectly coded as diphtheria.
Note 2 - due to toxigenic C. ulcerans, cases not notified.
Note 3 - due to toxigenic C. ulcerans.
Note 4 - due to toxigenic C. diphtheriae, case not notified.
Note 5 - an isolate from 1 notified case was not received; a second isolate was not Corynebacteria.
Note 6 - 3 isolates were non-toxigenic tox gene-bearing (NTTB) C. diphtheriae.
Note 7 - Corynebacterium spp. not isolated from 2 samples.
Note 8 - Corynebacterium spp. not isolated from 1 sample.
Note 9 - includes 1 NTTB C. diphtheriae.
Note 10 - Corynebacterium spp. not isolated from 11 samples.
Notifications, deaths and vaccine coverage in England and Wales from 1914 onward
Notes for figures 1 and 2:
- cases refers to notifications only (not laboratory confirmed) up to 1985. From 1986 onward, cases are confirmed by laboratory results
- death data is based on data from ONS where diphtheria is listed as cause of death; data may be incomplete for the current year
- from 2016 onwards, data is from England only
Figure 1. Diphtheria cases, deaths and vaccine coverage, England and Wales, 1914 to 2022
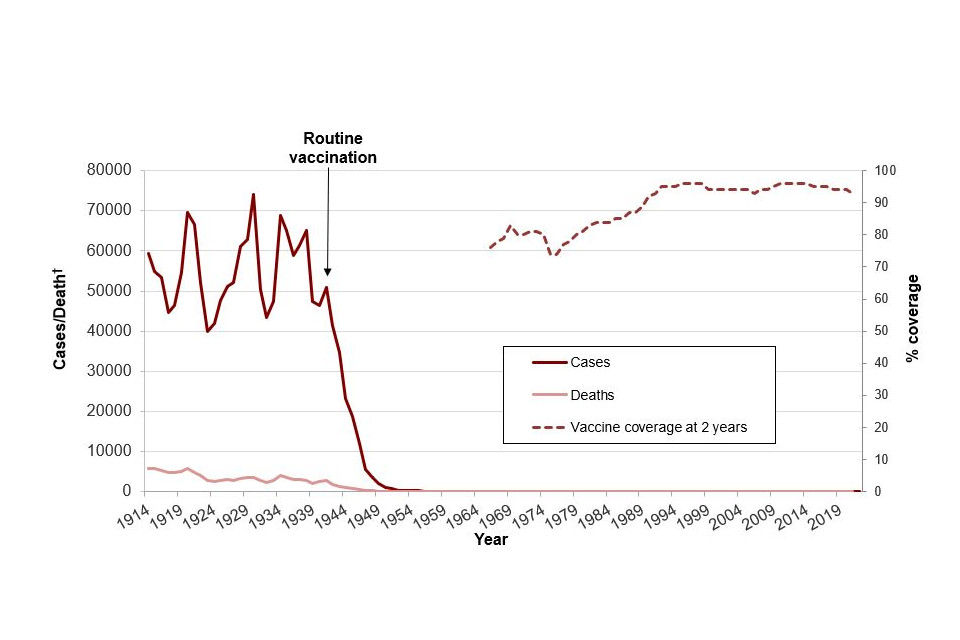
Figure 1 highlights the decrease in the number of diphtheria cases from 1942 when routine vaccination was introduced.
Figure 2. Diphtheria cases and deaths, England and Wales, 1914 to 2022
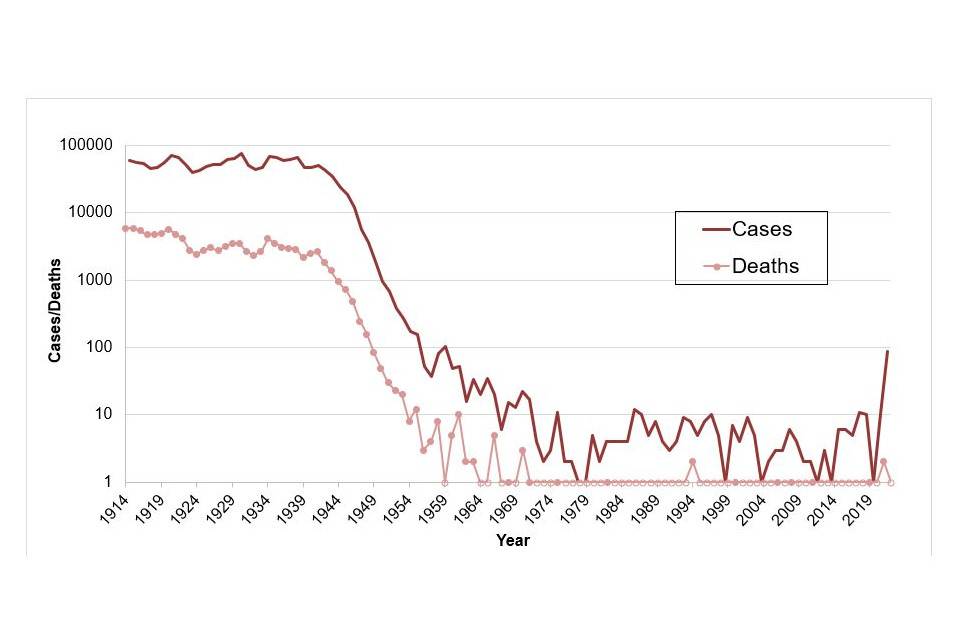
Figure 2 shows an increase in the number of diphtheria cases in 2022 compared to previous years.
Laboratory isolates of Corynebacterium diphtheriae and Corynebacterium ulcerans in England and Wales from 1986 onward
Pharyngeal or cutaneous diphtheria is caused by toxigenic strains of C. diphtheriae and by C. ulcerans. The table below shows the isolates received by the Respiratory and Vaccine Preventable Bacteria Reference Unit (RVPBRU) for toxigenicity testing. Numbers of isolates may vary from surveillance reports where cases are recorded against date of onset of symptoms.
Table 2. Laboratory isolates of C. diphtheriae and C. ulcerans in England and Wales, 1986 to 2022
From 2016 onwards, data is from England only.
For C. ulcerans (toxigenic and non-toxigenic), data was not routinely collected until 2009 onwards.
Testing for non-toxigenic tox gene-bearing C. diphtheriae started in 2014 .
| Year | C. diphtheriae: toxigenic | C. diphtheriae: non-toxigenic | C. ulcerans: toxigenic | C. ulcerans: non-toxigenic | NTTB C. diphtheriae | Total Corynebacteria Isolates |
|---|---|---|---|---|---|---|
| 1986 | 8 | 4 | 1 | no data | no data | 13 |
| 1987 | 2 | 8 | 2 | no data | no data | 12 |
| 1988 | 4 | 6 | 1 | no data | no data | 11 |
| 1989 | 6 | 12 | 2 | no data | no data | 20 |
| 1990 | 4 | 17 | 0 | no data | no data | 21 |
| 1991 | 1 | 11 | 2 | no data | no data | 14 |
| 1992 | 3 | 55 | 1 | no data | no data | 59 |
| 1993 | 5 | 51 | 4 | no data | no data | 60 |
| 1994 | 4 | 48 | 4 | no data | no data | 56 |
| 1995 | 1 | 137 | 4 | no data | no data | 142 |
| 1996 | 3 | 130 | 5 | no data | no data | 138 |
| 1997 | 5 | 178 | 5 | no data | no data | 188 |
| 1998 | 3 | 162 | 2 | no data | no data | 167 |
| 1999 | 0 | 255 | 2 | no data | no data | 256 |
| 2000 | 1 | 294 | 7 | no data | no data | 301 |
| 2001 | 0 | 205 | 3 | no data | no data | 209 |
| 2002 | 6 | 143 | 2 | no data | no data | 152 |
| 2003 | 3 | 147 | 2 | no data | no data | 152 |
| 2004 | 0 | 120 | 1 | 2 | no data | 144 |
| 2005 | 0 | 102 | 2 | 2 | no data | 116 |
| 2006 | 1 | 70 | 4 (see note 1) |
1 | no data | 103 |
| 2007 | 0 | 77 | 2 | 1 | no data | 90 (see note 2) |
| 2008 | 2 | 67 | 5 (see note 3) |
1 | no data | 93 |
| 2009 | 1 | 33 | 2 | 4 | no data | 45 |
| 2010 | 2 | 44 | 1 | 1 | no data | 53 |
| 2011 | 0 | 31 | 2 | 0 | no data | 37 |
| 2012 | 0 | 49 | 1 | 2 | no data | 53 |
| 2013 | 3 | 46 | 0 | 0 | no data | 50 |
| 2014 | 0 | 62 | 2 (see note 4) |
2 (see note 4) |
5 | 70 |
| 2015 | 3 | 44 | 3 | 1 | 1 | 52 (see note 2) |
| 2016 | 3 | 51 | 3 (see note 4) |
1 | 0 | 58 |
| 2017 | 5 (see note 5) |
68 | 2 (see note 4) |
4 | 2 (see note 6) |
81 |
| 2018 | 8 | 85 | 5 (see note 1) |
2 | 2 | 102 |
| 2019 | 0 | 70 | 17 (see note 7) |
6 (see note 1) |
2 | 95 |
| 2020 | 0 | 22 | 4 (see note 8) |
1 | 1 | 28 |
| 2021 | 3 | 19 | 11 (see notes 6 and 9) |
6 (see note 1) |
1 | 40 |
| 2022 | 81 | 106 | 34 (see note 10) |
17 (see note 11) |
1 | 239 |
Note 1 - includes 2 isolates from animals.
Note 2 - includes 1 non-toxigenic C. pseudotuberculosis isolate.
Note 3 - includes 1 isolate which was previously identified as toxigenic C. pseudotuberculosis.
Note 4 - includes one isolate from an animal.
Note 5 - includes 1 case with onset date in 2016, but tested in 2017.
Note 6 - includes 2 isolates from 1 individual.
Note 7 - includes 7 isolates from animals.
Note 8 - includes 3 isolates from animals; 1 contact of a human case from 2019.
Note 9 - includes 4 isolates from animals.
Note 10 - includes 20 isolates from animals.
Note 11 - includes 9 isolates from animals.
Contact
For queries relating to this document, please contact [email protected].
-
Classic respiratory diphtheria: a patient with an upper respiratory tract illness characterised by sore throat, low grade fever and an adherent membrane of the tonsils, pharynx or nose. Many clinicians will not have seen a classical presentation of diphtheria with a membrane. Clinical assessment of the likelihood of C. diphtheriae should include consideration of the likely source, with increased risk associated with recent travel from a diphtheria endemic country or over land travel to the UK along a migrant route with periods of stay in a migrant camp. ↩
