Group A streptococcal infections: update on seasonal activity in England, 2021 to 2022
Updated 20 September 2022
Applies to England
Main points
Notifications and GP consultations of scarlet fever in England are higher in 2022 compared with the past 2 years and have remained elevated later in the season than expected. Notifications of invasive group A streptococcus (iGAS) disease followed a similar trend and remain higher than expected for this time of year. Although the iGAS season total is below average compared to the past 5 years, relatively higher levels in children are noted. The unusual seasonal pattern is a likely result of the withdrawal of measures implemented during the coronavirus (COVID-19) pandemic to reduce transmission. The unusual seasonal patterns may continue in the near future.
Given the potential for severe presentations in children, it remains important that scarlet fever cases are treated promptly with antibiotics to limit further spread, and reduce risk of potential complications in cases and their close contacts. Due to these uncommon but potentially severe complications, clinicians (and health protection teams (HPTs)) should continue to be mindful of potential increases in invasive disease and maintain a high degree of clinical suspicion when assessing patients, particularly those with preceding chickenpox or close contacts of scarlet fever.
As per national guidance on GOV.UK, prompt notification of scarlet fever cases and outbreaks to local UK Health Security Agency (UKHSA) HPTs, obtaining throat swabs (prior to commencing antibiotics) when there is uncertainty about the diagnosis, and exclusion of cases from school or work until 24 hours of antibiotic treatment has been received, remain essential tools to limit spread.
Scarlet fever
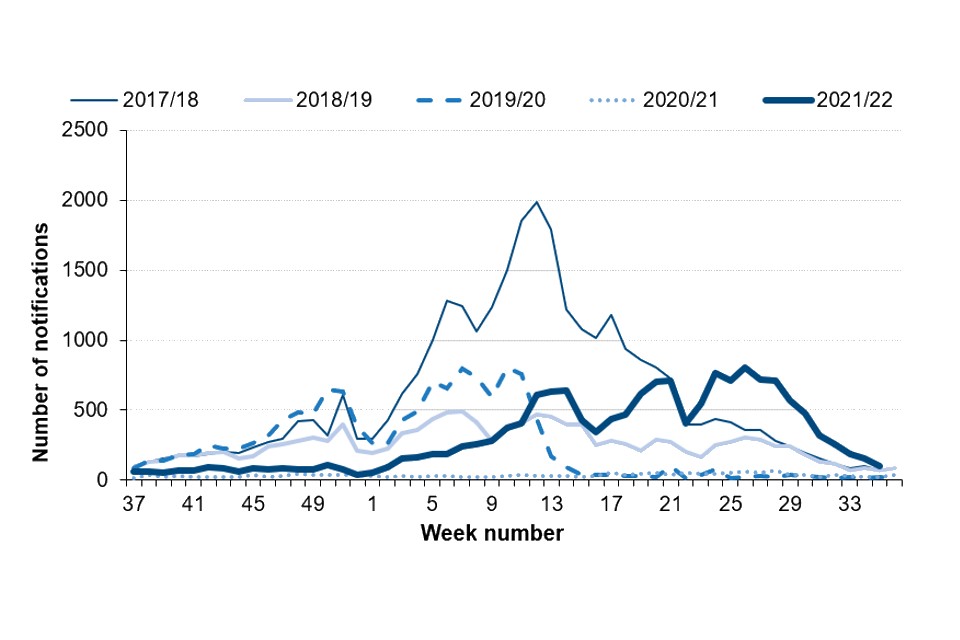
After low levels of activity last season (2020 to 2021) and at the start of the current season (2021 to 2022), scarlet fever notifications in England increased through spring and remained elevated through the summer (Figure 1). Notifications are currently higher than expected; however, larger week-on-week reductions were recorded during August (weeks 30 to 34).
A total of 15,894 notifications of scarlet fever have been received to date this season (week 37 of 2021 to week 35 of 2022), peaking in week 26 with 805 notifications. This compares with 1,791 notifications recorded across the 2020 to 2021 season (a peak of 62 notifications in week 26), and an average of 14,704 (range 1,731 to 30,681) for this same period (weeks 37 to 35) in the previous 5 years. In the 3 seasons prior to the COVID-19 pandemic, the season peaked in week 12 (2017 to 2018), week 7 (2018 to 2019) and week 10 (2019 to 2020).
Figure 1. Weekly scarlet fever notifications in England, by season, 2017 to 2018 onwards
Regional variations in scarlet fever notifications to date this season have been considerable, ranging between 16.1 (South West) and 54.3 (North East) per 100,000 population (Table 1). After the North East, the highest observed rates were in the North West (53.5), Yorkshire and the Humber (43.6) and the East Midlands (37.8) regions.
Table 1. Counts and rate per 100,000 population of scarlet fever and iGAS notifications in England: week 37 of 2021 to week 35 of 2022
| Region | Number of cases of scarlet fever | Rate of scarlet fever | Number of cases of iGAS | Rate of iGAS |
|---|---|---|---|---|
| East of England | 1,355 | 20.2 | 183 | 2.7 |
| East Midlands | 1,837 | 37.8 | 133 | 2.7 |
| London | 1,472 | 16.4 | 199 | 2.2 |
| North East | 1,456 | 54.3 | 121 | 4.5 |
| North West | 3,940 | 53.5 | 282 | 3.8 |
| South East | 1,473 | 16.5 | 231 | 2.6 |
| South West | 885 | 16.1 | 174 | 3.2 |
| West Midlands | 1,065 | 17.9 | 199 | 3.3 |
| Yorkshire and the Humber | 2,411 | 43.6 | 244 | 4.4 |
| England | 15,894 | 28.1 | 1,766 | 3.1 |
Invasive group A streptococcal infection
As with scarlet fever, after low levels of activity at the start of the season, iGAS notifications in England increased through spring and have remained elevated during the summer. Notifications are currently higher than expected; however, reductions have been recorded during August (weeks 30 to 34).
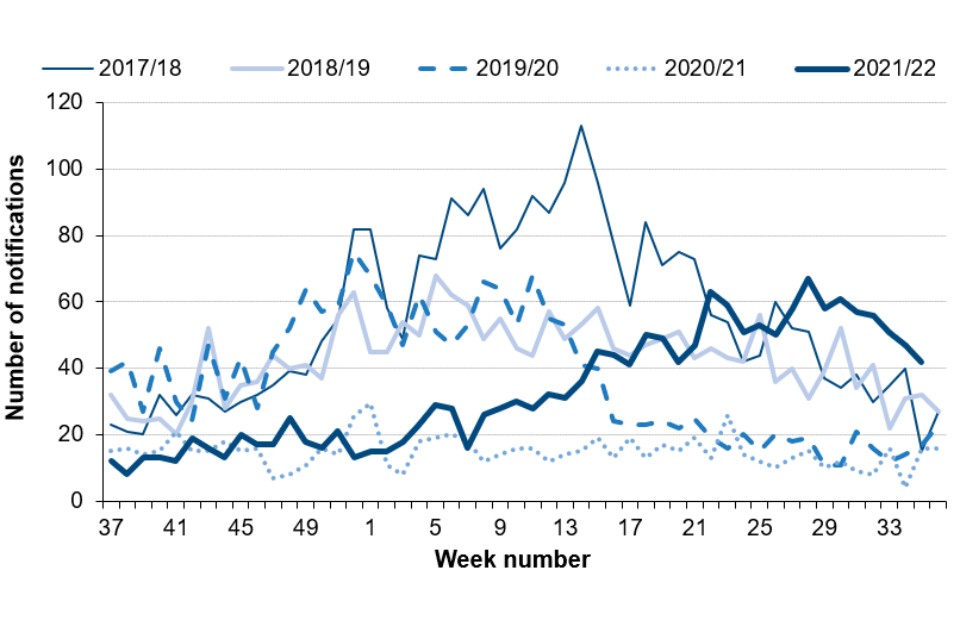
So far this season (week 37 of 2021 to 35 of 2022), there have been 1,699 notifications of iGAS disease reported through laboratory surveillance, peaking with 67 notifications in week 26. Laboratory notifications of iGAS are higher compared with last season (757, peaking in week 23 with 26 notifications), but lower than the average (1,937) for the previous 5 years (range 757 to 2,848; Figure 2). Prior to the COVID-19 pandemic, the seasonal peak was earlier in the season, peaking with 113 in week 14 in 2017 to 2018, week 5 in 2018 to 2019 (68 notifications) and week 52 in 2019 to 2020 (75 notifications, although a large reduction midway through the season was noted, coinciding with the first wave of the COVID-19 pandemic).
In line with the scarlet fever notification data, during the current season to date, the highest rates so far were reported in the North East region (4.5 per 100,000 population), followed by the Yorkshire and Humber (4.4 per 100,000) and North West (3.8 per 100,000) regions (Table 1).
Figure 2. Weekly laboratory notifications of iGAS, England, by season, 2017 to 2018 onwards
The iGAS rate per 100,000 population by age group is presented in Figure 3. In the current season (2021 to 2022) the highest rate was in the <1 year age group and the ≥75 years age group (9.3 per 100,000 for both), followed by the 1 to 4 years age group (8.2 per 100,000). This pattern aligns with what is normally reported.
Figure 3. Rate per 100,000 population iGAS notifications in England by age group, weeks 37 to 35
Note: in this graph, the ‘pre-pandemic period’ is the average rate per 100,000 population recorded in the 3 pre-pandemic seasons: 2016 to 2017, 2017 to 2018, and 2018 to 2019. The ‘pandemic season’ is the average rate recorded in the 2019 to 2020 season, and in the 2020 to 2021 season to date.
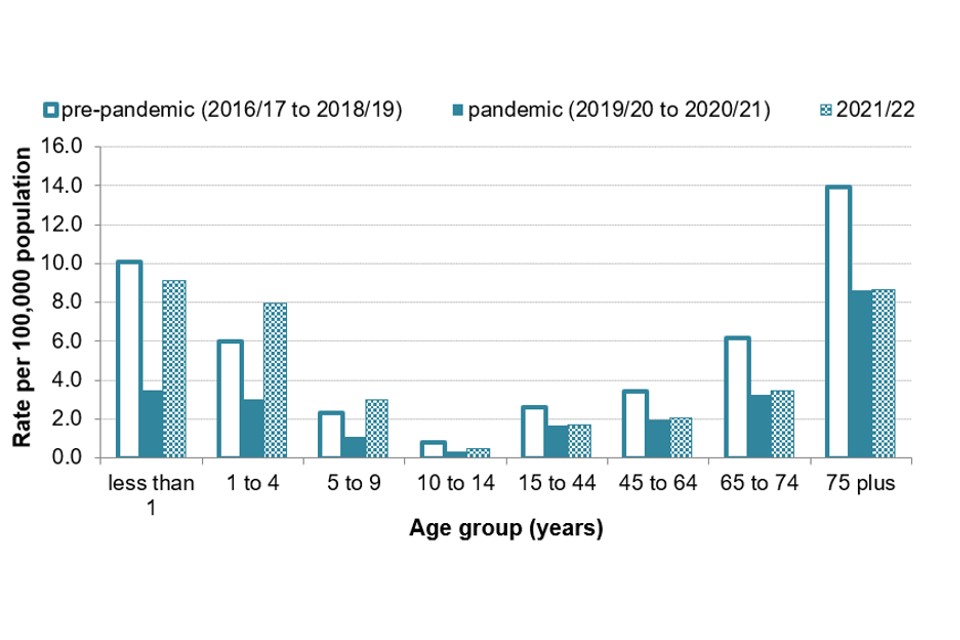
For the current season (2021 to 2022) to date, rates of iGAS infection in infants (less than 1) have been similar to the pre-pandemic average (10.1 per 100,000); however, the rate in the 1 to 4 years age group has been slightly higher compared with the pre-pandemic average (6.0 per 100,000). In age groups above 10 years, rates of iGAS infection have been similar to the pandemic seasons but lower than pre-pandemic seasons.
The median age of patients with iGAS infection was 51 years (range <1 year to 102 years), which is lower than the range seen at this point in the preceding 5 seasons (56 to 59 years); 21% of iGAS infections reported this season are in children (<10 years), higher than the range seen for the past 5 seasons (11% to 13%, excluding the 2020 to 2021 season which recorded only 4% in children).
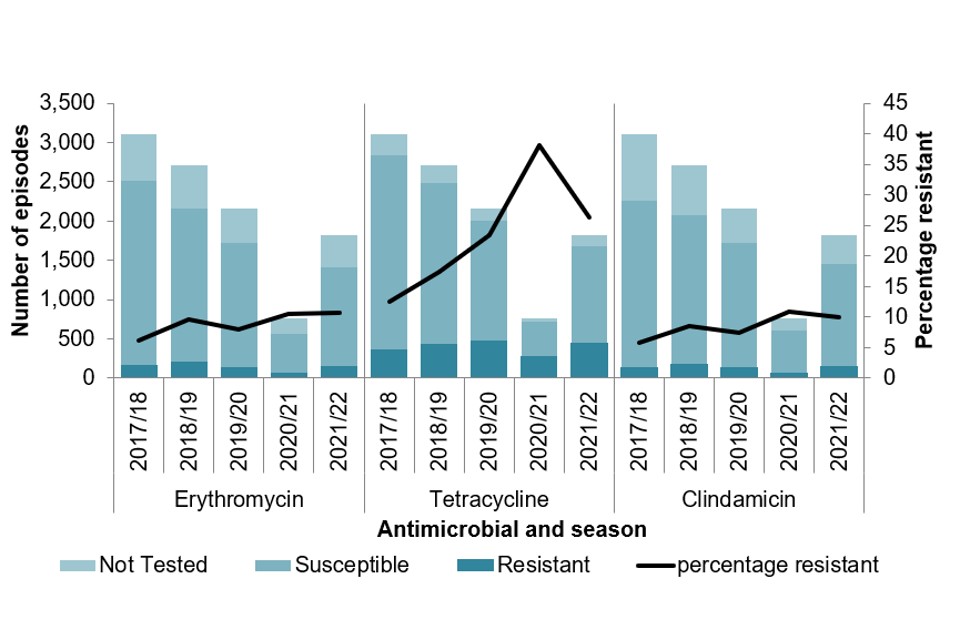
Antimicrobial susceptibility results from routine laboratory surveillance so far this season (September 2021 to August 2022) indicate erythromycin resistance in 11% of GAS sterile site isolates; this is following a gradual increasing trend in resistance, from 6% in 2017 to 2018 (Figure 4). There has also been an increasing trend in tetracycline resistance, from 11% to 26% resistant between 2017 to 2018 and 2021 to 2022, although this season saw a decrease from the 2020 to 2021 season (38%). Susceptibility testing of iGAS isolates against clindamycin demonstrated 10% resistant at this point in the season (compared with 11% last season), and isolates remained universally susceptible to penicillin.
Figure 4. Antimicrobial resistance to key antibiotics in iGAS episodes, England, by season, 2017 to 2018 onwards
Analysis of reference laboratory iGAS isolate submissions indicate a diverse range of emm gene sequence types identified between January and August 2022. The results indicate the emm 1 are the most common (24% of referrals), followed by emm 12 (19%), emm 89 (8%), and emm 108 and emm 33 (each 5%). In children (aged <15 years) emm 12 and emm 1 have dominated, accounting for 40% and 35% respectively.
During 2021, emm 89 was the most frequently identified (13%), followed by emm 108 (12%) then emm 66 (11%).
Discussion
The rate of scarlet fever notifications and GP consultations was low in the early part of the season, with a subsequent increase seen in spring and remaining elevated through summer, when reductions would have been typically expected. The rate of iGAS infection notifications followed a similar trend, increasing in spring and remaining elevated through summer. In children under 10 years, the rate of iGAS infection has been similar or slightly higher than levels reported in the years preceding the COVID-19 pandemic but substantially higher than the past 24 months. The rate of iGAS has declined through August, though it remains above expected.
This summer elevation in scarlet fever, with loss of typical seasonality, is likely to be a result of measures associated with the COVID-19 pandemic, including those to reduce transmission in schools and wider society, such as limiting mixing and use of masks (1). This could have led to differing population susceptibility. The elevated iGAS levels in children compared to the period when these pandemic control measures were in place is likely to be a consequence of the heightened scarlet fever activity given the crossover of strains associated in both presentations (2, 3). This is further supported by the regional differences in rates of both – which showed some association between the 2 presentations. With uncertainty around expected levels, it is possible that further increases following the start of the academic year could be seen.
Prompt treatment of scarlet fever with antibiotics is recommended to reduce risk of possible complications and limit onward transmission. Renewed messaging to encourage contact with GP practices for clinical assessment of patients with specific symptoms (for example rash), should be considered. GPs and other frontline clinical staff are reminded of the increased risk of invasive disease among household contacts of scarlet fever cases (4, 5).
Clinicians, microbiologists and HPTs should continue to be mindful of potential increases in invasive disease and maintain a high index of suspicion in relevant patients as early recognition and prompt initiation of specific and supportive therapy for patients with iGAS infection can be life-saving.
Although penicillin resistance has not been detected in England to date, the percentage of iGAS specimens that are resistant to other key antibiotics, namely erythromycin, clindamycin and tetracycline, has been increasing over the last few seasons. GPs and other clinical staff should consider this when treating patients with suspected GAS infection, particularly patients unable to tolerate penicillin-based regimes.
Invasive disease isolates and superficial isolates from suspected clusters or outbreaks should be submitted to:
The Staphylococcus and Streptococcus Reference Section
Antimicrobial Resistance and Healthcare Associated Infections (AMRHAI) unit
UK Health Security Agency
61 Colindale Avenue
London NW9 5HT
Prepared by: Rebecca Guy, Ashley Sharp, Juliana Coelho, Colin Brown and Theresa Lamagni.
For queries relating to this document, please contact [email protected]
References
1. Chudasama D and others (2021). ‘Surge in SARS-CoV-2 transmission in school-aged children and household contacts, England, August to October 2021’, Eurosurveillance: volume 26, number 48
2. 1. Chalker V, Jironkin A, Coelho J, Al-Shahib A, Platt S, Kapatai G, and others (2017). ‘Genome analysis following a national increase in scarlet fever in England 2014’. BMC Genomics. volume 18, number 1, page 224
3. Al-Shahib A, Underwood A, Afshar B, Turner CE, Lamagni T, Sriskandan S, and others (2016). ‘Emergence of a novel lineage containing a prophage in emm/M3 group A Streptococcus associated with upsurge in invasive disease in the UK’. mGen volume 2, number 11 (e000097)
4. Lamagni T and others (2018). ‘Resurgence of scarlet fever in England, 2014 to 2016: A population-based surveillance study’, Lancet Infectious Diseases: volume 18, number 2, pages 180 to 187
5. Watts V and others (2019). ‘Increased risk for invasive group A Streptococcus disease for household contacts of scarlet fever cases, England, 2011 to 2016’, Emerging Infectious Diseases: volume 25, number 3, pages 529 to 537
