Group A streptococcal infections: report on seasonal activity in England, 2022 to 2023
Updated 29 June 2023
Applies to England
Notifications and GP consultations of scarlet fever in England are higher than normal for this point in the season, after remaining elevated later in the previous season than expected.
Notifications of invasive group A streptococcus (iGAS) disease are following a similar trend and are slightly higher than expected for this time of year. The relatively higher rates of iGAS in children are noted and may reflect increases in respiratory viruses.
Given the potential for severe presentations in children, it remains important that scarlet fever cases are treated promptly with antibiotics to limit further spread and reduce risk of potential complications in cases and their close contacts. Due to these uncommon but potentially severe complications, clinicians and health protection teams (HPTs) should continue to be mindful of potential increases in invasive disease and maintain a high degree of clinical suspicion when assessing patients, particularly those with preceding viral infection (including chickenpox) or close contacts of scarlet fever.
As per national guidance, prompt notification of scarlet fever cases and outbreaks to local UK Health Security Agency (UKHSA) HPTs, obtaining throat swabs (prior to commencing antibiotics) when there is uncertainty about the diagnosis, and exclusion of cases from school or work until 24 hours of antibiotic treatment has been received, remain essential tools to limit spread.
Scarlet fever
Following higher than expected scarlet fever activity in the summer in England, with a drop during August, notifications during the early part of the current season (2022 to 2023; seasons are defined from mid-September to mid-September) are increasing again and remain above what is normally seen at this time of year (Figure 1).
A total of 4,622 notifications of scarlet fever were received from week 37 to 46 this season (2022 to 2023) in England, with 851 notifications received in week 46. This compares with an average of 1,294 (range 258 to 2,008) for this same period (weeks 37 to 46) in the previous 5 years.
Figure 1. Weekly scarlet fever notifications in England, by season, 2017 to 2018 onwards
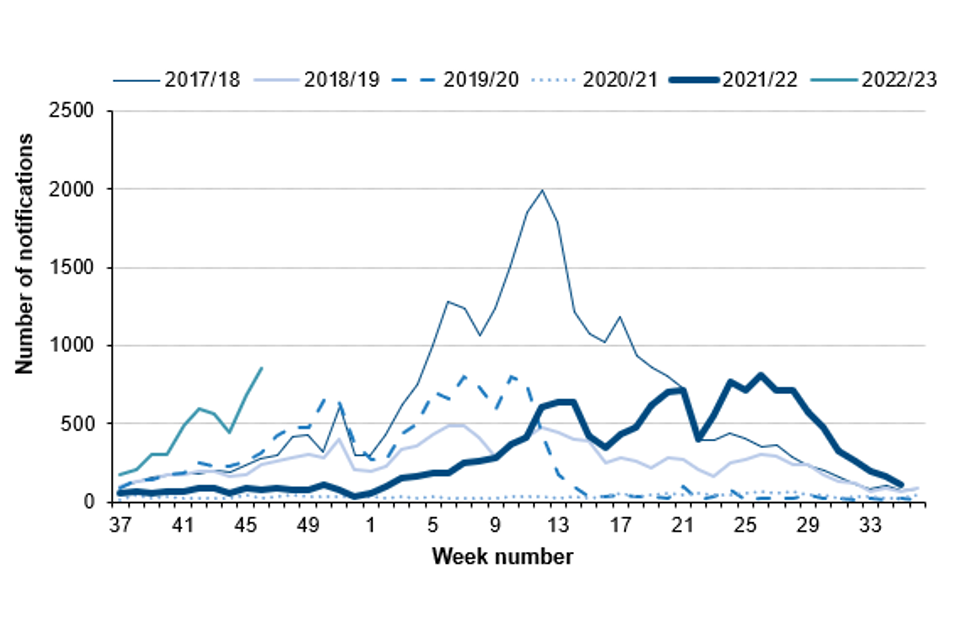
Scarlet fever notifications to date this season showed considerable variation across England, ranging between 3.9 (London) and 13.0 (North West) per 100,000 population (Table 1).
Table 1. Number and rate per 100,000 population of scarlet fever and iGAS notifications in England: week 37 to week 46 of the 2022 to 2023 season
| Region | Number of cases of scarlet fever | Rate of scarlet fever | Number of cases of iGAS | Rate of iGAS |
|---|---|---|---|---|
| East of England | 436 | 6.5 | 39 | 0.6 |
| East Midlands | 578 | 11.9 | 40 | 0.8 |
| London | 347 | 3.9 | 71 | 0.8 |
| North East | 234 | 8.7 | 26 | 1.0 |
| North West | 957 | 13.0 | 74 | 1.0 |
| South East | 638 | 7.1 | 85 | 1.0 |
| South West | 404 | 7.3 | 49 | 0.9 |
| West Midlands | 418 | 7.0 | 51 | 0.9 |
| Yorkshire and the Humber | 610 | 11.0 | 75 | 1.4 |
| England | 4,622 | 8.2 | 510 | 0.9 |
Invasive group A streptococcal infection
As with scarlet fever, during the latter part of last season (2021 to 2022), the levels of iGAS notifications in England were higher than expected (Figure 1). Laboratory notifications of iGAS so far this season (weeks 37 to 46, 2022 to 2023) are higher than expected. So far this season there have been 509 notifications of iGAS disease reported through laboratory surveillance in England, with a weekly high of 73 notifications in week 46.
Laboratory notifications of iGAS are higher than recorded over the last 5 seasons (average 248, range 142 to 357 notifications; Figure 2).
Figure 2. Weekly laboratory notifications of iGAS, England, by season, 2017 to 2018 onwards
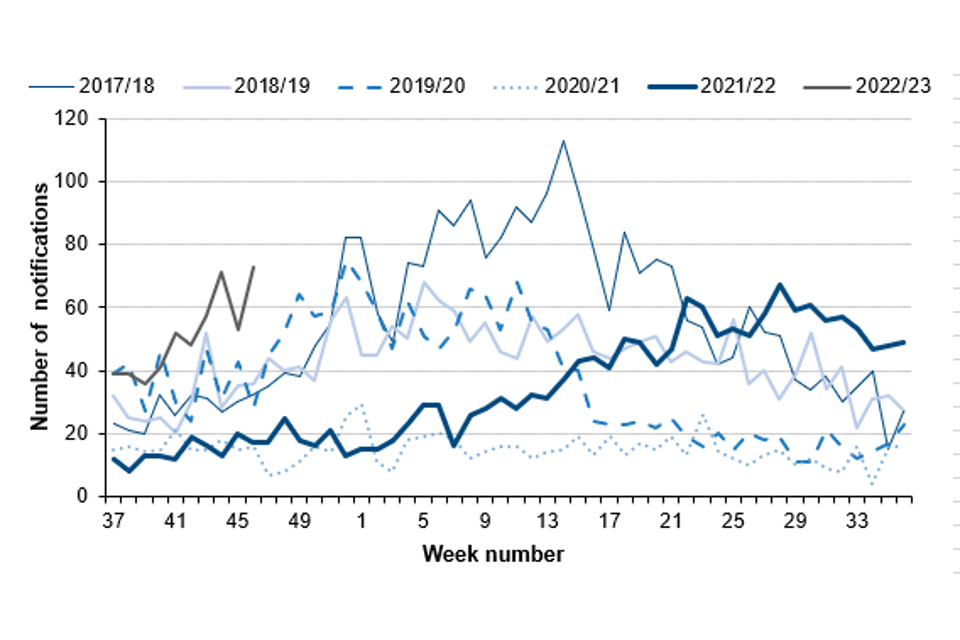
During the current season to date, the highest rates so far were reported in the Yorkshire and Humber region (1.4 per 100,000 population), followed by the North East, South East and North West regions (each 1.0 per 100,000; Table 1). The highest rate was in those aged 75 years and over (2.4 per 100,000), followed by the 1 to 4 years age group (2.3 per 100,000) and those aged 1 year and under (1.3 per 100,000).
The rate of iGAS at this point in the season is higher in all age groups compared with the pre-pandemic average (Table 2).
Table 2. Rate per 100,000 population of iGAS notifications in England by age group, weeks 37 to 46
Note: In this table, the ‘pre-pandemic period’ is the average rate per 100,000 population recorded in the 3 pre-pandemic seasons: 2017 to 2018, 2018 to 2019 and 2019 to 2020. The ‘pandemic’ rate is the average rate recorded in the 2020 to 2021 and 2021 to 2022 seasons.
| Age group (years) | Pre-pandemic (2017/18 to 2019/20) | Pandemic (2020/21 to 2021/22) | 2022 to 2023 |
|---|---|---|---|
| Under 1 | 1.1 | 0.2 | 1.3 |
| 1 to 4 | 0.5 | 0.2 | 2.3 |
| 5 to 9 | 0.3 | 0.1 | 1.1 |
| 10 to 14 | 0.1 | 0.3 | 0.2 |
| 15 to 44 | 0.4 | 0.2 | 0.5 |
| 45 to 64 | 0.5 | 0.2 | 0.6 |
| 65 to 74 | 0.7 | 0.3 | 1.3 |
| 75 and over | 1.9 | 1.0 | 2.4 |
The median age of patients with iGAS infection was 50 years (range 1 year and under, to 102 years), slightly lower than the range seen at this point in the preceding 5 seasons (age 54 to 57 years); 21% of iGAS infections reported so far this season are in children (age 10 years and under), higher than the range seen for the past 5 seasons (5% to 11%).
So far this season 5 deaths have been recorded within 7 days of an iGAS infection diagnosis (from any cause) in children under 10 years of age. This compares with 4 deaths in the same period in the 2017 to 2018 (pre-pandemic) season, our last high season for GAS infection.
Antimicrobial susceptibility results from routine laboratory surveillance so far this season indicate tetracycline resistance in 25% of GAS sterile site isolates; this is lower than at this point last season (45%). Susceptibility testing of iGAS isolates against erythromycin indicated 7% were found resistant (compared with 19% last season), and for clindamycin, 7% were resistant at this point in the season (16% last season). Isolates remained universally susceptible to penicillin.
Analysis of reference laboratory iGAS isolate submissions indicate a diverse range of emm gene sequence types identified between October and November 2022. The results indicate the emm 1 are the most common (24% of referrals), followed by emm 12 (20%), emm 89 (8%), emm 108 and emm 33 (each 5%). In children (aged 15 years and under) emm 12 and emm 1 have dominated in 2022, accounting for 39% and 35% respectively. In contrast, during 2021, emm 89 was the most frequently identified (13%), followed by emm 108 (12%), then emm 66 (11%).
Discussion
There has been a steep increase in scarlet fever notification and GP consultations early in the 2022 to 2023 season which is steeper than would be expected at this time of the year. The rate of iGAS infection notifications is following a similar but less pronounced increase, with weekly incidence trending slightly above what would be expected at this point in the season.
In children under 10 years, the rate of iGAS infection has been higher than levels reported in the years preceding the COVID-19 pandemic but substantially higher than the past 2 years. Investigations are underway following reports of an increase in lower respiratory tract GAS infections, particularly empyema, in children over the past few weeks.
The elevated iGAS levels in children compared to the period when these pandemic control measures were in place is likely to be a consequence of the heightened scarlet fever activity given the crossover of strains associated in both presentations (1, 2).
Prompt treatment of scarlet fever with antibiotics is recommended to reduce risk of possible complications and limit onward transmission. Public health messaging to encourage contact with NHS 111 and/or GP practices for clinical assessment of patients with specific symptoms (for example, rash) is underway. GPs and other frontline clinical staff are reminded of the increased risk of invasive disease among household contacts of scarlet fever cases (3, 4).
Clinicians should continue to be mindful of potential increases in invasive disease and maintain a high index of suspicion in relevant patients and provide safety netting advice as appropriate, as early recognition and prompt initiation of specific and supportive therapy for patients with iGAS infection can be life-saving.
Relevant guidelines and information can be found on GOV.UK:
- Guidelines for the public health management of scarlet fever outbreaks in schools, nurseries and other childcare settings
- Scarlet fever: symptoms, diagnosis and treatment
- Guidelines for the management of close community contacts of invasive GAS cases and the prevention and control of GAS transmission in acute healthcare and maternity settings
- Weekly notifiable diseases reports are published each week for a timelier update
Invasive disease isolates and also non-invasive isolates from suspected clusters or outbreaks should be submitted to:
Staphylococcus and Streptococcus Reference Section
Antimicrobial Resistance and Healthcare Associated Infections (AMRHAI)
UK Health Security Agency
61 Colindale Avenue
London
NW9 5HT
References
1. Chalker V, Jironkin A, Coelho J, Al-Shahib A, Platt S, Kapatai G, and others (2017). ‘Genome analysis following a national increase in scarlet fever in England 2014’. BMC Genomics: volume 18 number 1, page 224
2. Al-Shahib A, Underwood A, Afshar B, Turner CE, Lamagni T, Sriskandan S, and others (2106). Emergence of a novel lineage containing a prophage in emm/M3 group A Streptococcus associated with upsurge in invasive disease in the UK’. mGen; volume 2 number 11
3. Lamagni T, and others (2018). ‘Resurgence of scarlet fever in England, 2014–16: a population based surveillance study’. The Lancet Infectious Diseases: volume 18, number 2, pages 180 to 187
4. Watts V, and others (2019). ‘Increased risk for Invasive Group A Streptococcus disease for household contacts of scarlet fever cases, England, 2011–2016’. Emerging Infectious Diseases: volume 25, number 3, pages 529 to 537
Acknowledgements
These reports would not be possible without the weekly contributions from microbiology colleagues in laboratories across England, without whom there would be no surveillance data.
The support from colleagues within UKHSA, and the AMRHAI Reference Unit in particular, is valued in the preparation of the report.
Feedback and specific queries about this report are welcome via [email protected]
