Group A streptococcal infections: second update on seasonal activity in England, 2022 to 2023
Updated 29 June 2023
Applies to England
Data to 11 December 2022.
Notifications and GP consultations of scarlet fever in England are higher than normal for this point in the season, after persisting later into the previous season.
Notifications of invasive group A streptococcus (iGAS) disease are following a similar trend with higher than expected levels for this time of year. Relatively high rates of iGAS in children are noted. This may reflect increases in respiratory viruses and high levels of group A streptococcus (GAS) circulating in children.
Medical practitioners have been alerted to this early increase in incidence and elevated iGAS infection in children. Given the potential for severe presentations, it remains important that scarlet fever cases are treated promptly with antibiotics to limit further spread and reduce risk of potential complications in cases and their close contacts. Interim clinical guidance on management of GAS infection has been issued to optimise diagnosis and treatment during this current increase in infection. Clinicians should continue to be alert to the severe complications of GAS and maintain a high degree of clinical suspicion when assessing patients, particularly those with preceding viral infection (including chickenpox) or close contacts of scarlet fever.
As per national guidance, prompt notification of scarlet fever cases and outbreaks to local UK Health Security Agency (UKHSA) HPTs, obtaining throat swabs (prior to commencing antibiotics) when there is uncertainty about the diagnosis, and exclusion of cases from school or work until 24 hours of antibiotic treatment has been received, remain essential tools to limit spread.
Data presented within this seasonal activity update is based on data available as at 14 December 2022 and goes up to 11 December 2022 (the end of week 49). An updated report will be published in a week on 22 December 2022. Weekly notifiable disease reports are published each week throughout the year to provide a regular update of scarlet fever notifications.
Key definitions are available at the end of the report.
Scarlet fever
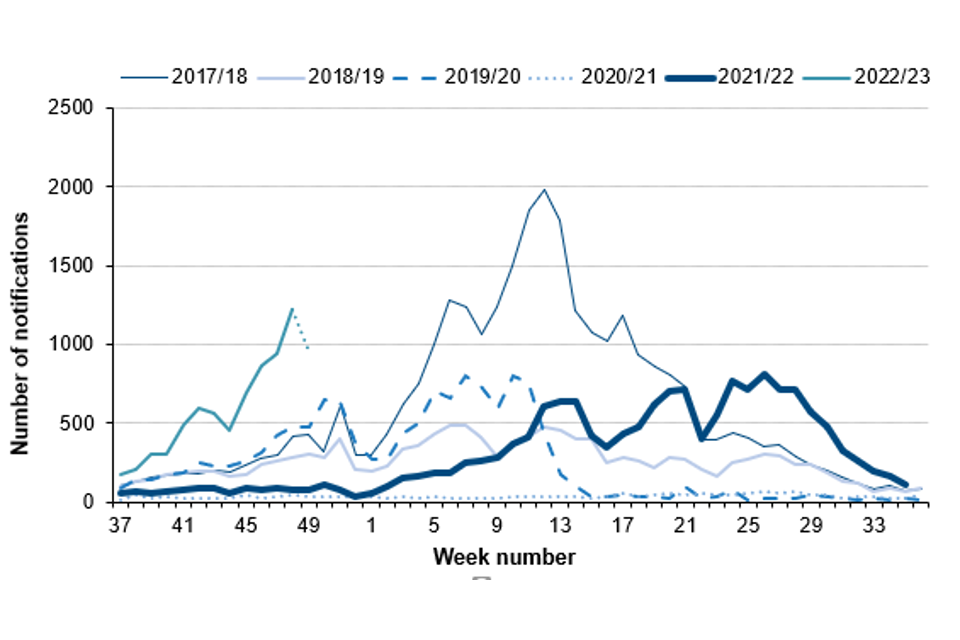
Following higher than expected scarlet fever activity during the early part of this summer in England, with a drop during August, notifications during the early part of the current season (2022 to 2023; seasons are defined from week 37 (mid-September) to week 36 (mid-September)) are increasing again and remain higher than expected for this time of year (Figure 1).
A total of 7,750 notifications of scarlet fever were received from week 37 to 49 this season (2022 to 2023) in England, with 1,221 notifications received so far for week 48. This compares with an average of 2,040 (range 370 to 3,394) for this same period (weeks 37 to 49) in the previous 5 years. While high for this point in the season, the weekly notifications are lower than the weekly totals seen during the normal pre-pandemic peak season (February to March) where peak weekly total was 1,988 in week 12 during the 2017 to 2018 season (19 March 2018 to 25 March 2018 (Figure 1)).
Figure 1. Weekly scarlet fever notifications in England, by season, 2017 to 2018 onwards (weeks 37 to 49)
Note: In this graph the 2022 to 2023 season goes up to week 49 (11 December 2022). Recent weeks in the current season may change as further notifications are received, represented by a dotted line between week 48 and 49.
Scarlet fever notifications to date this season showed considerable variation across England, ranging between 8.1 (London) and 28.9 (North East) per 100,000 population (Table 1); while this may represent differential disease transmission it may also relate to differential notification practices by clinicians.
Table 1. Number and rate per 100,000 population of scarlet fever and iGAS notifications in England: week 37 to week 49 of the 2022 to 2023 season
| Region | Number of cases of scarlet fever | Rate of scarlet fever | Number of cases of iGAS | Rate of iGAS |
|---|---|---|---|---|
| East of England | 910 | 13.6 | 68 | 1.0 |
| East Midlands | 846 | 17.4 | 68 | 1.4 |
| London | 728 | 8.1 | 101 | 1.1 |
| North East | 775 | 28.9 | 43 | 1.6 |
| North West | 1,380 | 18.7 | 109 | 1.5 |
| South East | 1,311 | 14.7 | 156 | 1.7 |
| South West | 479 | 8.7 | 99 | 1.8 |
| West Midlands | 565 | 9.5 | 74 | 1.2 |
| Yorkshire and the Humber | 756 | 13.7 | 118 | 2.1 |
| England | 7,750 | 13.7 | 836 | 1.5 |
Invasive group A streptococcal infection
Laboratory notifications of iGAS so far this season (weeks 37 to 49, 2022 to 2023) are higher than expected (Figure 2). So far this season there have been 836 notifications of iGAS disease reported through laboratory surveillance in England, with a weekly high of 101 notifications in week 47 (21 to 27 December 2022). Laboratory notifications of iGAS infection are higher than recorded over the last 5 seasons for the same weeks (average 345, range 186 to 516 notifications; Figure 2).
Figure 2. Weekly laboratory notifications of iGAS, England, by season, 2017 to 2018 onwards (weeks 37 to 49)
Note: In this graph, the most recent weeks of the 2022 to 2023 season are expected to increase due to lags in reporting timelines from laboratories. The decline in the most recent week (week 49) should not be interpreted as an actual drop in laboratory notifications: it is therefore represented by a dotted line between week 48 and 49.
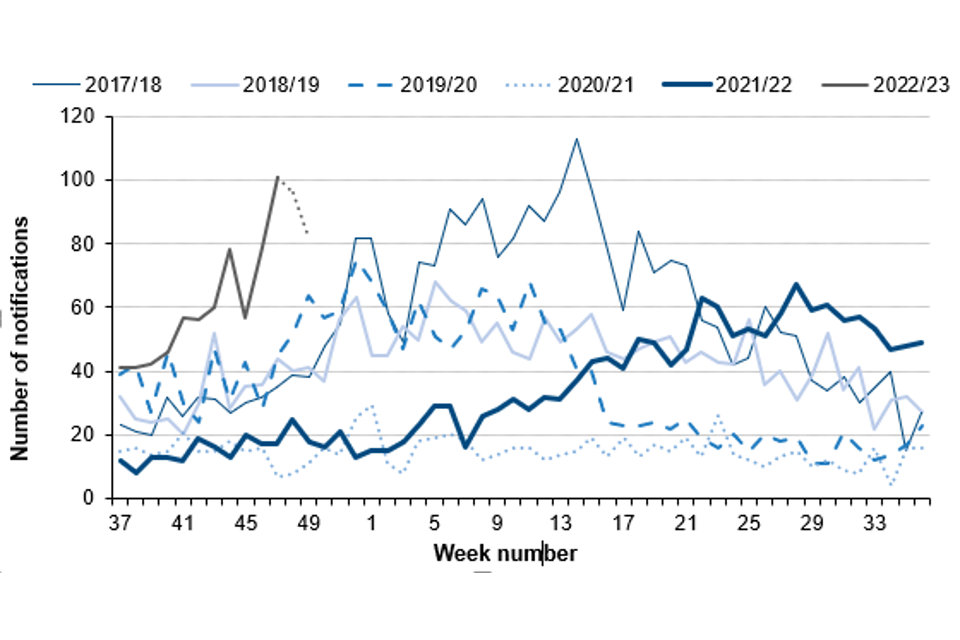
While high for this point in the season, the weekly laboratory notifications are lower than the weekly totals seen during the normal pre-pandemic peak season (March to April) where the peak weekly total was 113 in week 14 during the 2017 to 2018 season (2 April 2018 to 8 April 2018; Figure 2). Further increases may however be seen in the coming weeks.
During the current season to date, the highest rates so far were reported in the Yorkshire and Humber region (2.1 per 100,000 population), followed by the South West region (1.8 per 100,000) and South East region (1.7 per 100,000; Table 1).
The highest rate was in the 1 to 4 years age group (4.2 per 100,000), followed by those aged 75 years and over (3.7 per 100,000) and the under-1-year age group (2.8 per 100,000; Table 2).
Table 2. Rate per 100,000 population of iGAS notifications in England by age group, weeks 37 to 49 in the 2022 to 2023 season versus the 2017 to 2018 season
Note: In this table the current 2022 to 2023 season covers weeks 37 to 49, whereas the 2017 to 18 season data covers the full season, weeks 37 to 36.
| Age group (years) | 2022 to 2023 season (weeks 37 to 49): number of cases | 2022 to 2023 season (weeks 37 to 49): rate per 100,000 population | 2017 to 2018 (full season): number of cases | 2017 to 2018 (full season): rate per 100,000 population |
|---|---|---|---|---|
| Aged 1 year and under | 17 | 2.8 | 80 | 12.5 |
| 1 to 4 | 111 | 4.2 | 194 | 7.2 |
| 5 to 9 | 74 | 2.1 | 117 | 3.3 |
| 10 to 14 | 15 | 0.4 | 40 | 1.2 |
| 15 to 44 | 184 | 0.9 | 633 | 3.0 |
| 45 to 64 | 141 | 1.0 | 625 | 4.4 |
| 65 to 74 | 113 | 2.0 | 480 | 8.7 |
| 75 and over | 181 | 3.7 | 792 | 17.0 |
| Total | 836 | 1.5 | 2,967 | 5.3 |
The median age of patients with iGAS infection so far this season was 47 years (range 1 year and under, to 102 years), slightly lower than the range seen at this point in the preceding 5 seasons (age 54 to 57.5 years); 24% of iGAS infections reported so far this season are in children (aged 10 years and under), higher than the range seen for the past 5 seasons (4% to 12%). There have been 213 iGAS reports in children aged under 18 years in the season to date.
So far this season 74 deaths have been recorded within 7 days of an iGAS infection diagnosis (from any cause), with 39% (n=29) of the recorded deaths being in those aged 75 years and over, and 17% (n=12) in children aged 10 years and under (Table 3). The case fatality rate (CFR) to date remains comparable this season to recent seasons. Elevations in rates of iGAS infection in children in this early part of this season have resulted in an increased number of deaths over a relatively short period, with 16 deaths in children aged under 15 in weeks 37 to 49.
Antimicrobial susceptibility results from routine laboratory surveillance so far this season indicate tetracycline resistance in 17% of GAS sterile site isolates; this is lower than at this point last season (46%). Susceptibility testing of iGAS isolates against erythromycin indicated 6% were found resistant (compared with 20% last season) and, for clindamycin, 5% were resistant at this point in the season (16% last season). Isolates remained universally susceptible to penicillin.
Analysis of iGAS isolate typing data continues to indicate a diverse range of emm gene sequence types identified this season. The results indicate emm 1 was the most common (37% of referrals), followed by emm 12 (17%), emm 89 (5%), emm 108 and emm 77 (each 4%). In children (aged <15 years) emm 1 and emm 12 have dominated this season, accounting for 58% and 24% respectively.
Table 3. Case fatality rate (%) for deaths (all causes) within 7 days of an iGAS specimen, by age group in England for the current season and the previous 5 seasons
Notes: The total may include notifications where the age was unknown. The case fatality rate (CFR) is the percentage of deaths within 7 days of iGAS infection diagnosis for cases where follow-up has been possible. CFR should be interpreted with caution given the small numbers involved. The current season data (2022 to 2023) covers weeks 37 to 49 (12 September 2022 to 11 December 2022). The prior season’s data covers the whole season (weeks 37 to 36). ‘Pandemic seasons’ presents data for the 2019 to 2020 and 2020 to 2021 seasons combined.
| Age group (years) | 2017 to 2018 season % CFR | 2018 to 2019 season % CFR | Pandemic seasons (2019/2020 and 2020/2021) % CFR | 2021 to 2022 season % CFR | 2022 to 2023 season (weeks 37-49) % CFR | 2022 to 2023 season: number of deaths (all causes) within 7 days of iGAS |
|---|---|---|---|---|---|---|
| Aged 1 year and under | 5.6% | 2.1% | 7.7% | 3.8% | 0.0% | 0 |
| 1 to 4 | 4.7% | 6.1% | 9.0% | 5.9% | 7.1% | 7 |
| 5 to 9 | 9.9% | 4.6% | 2.7% | 10.6% | 7.2% | 5 |
| 10 to 14 | 7.9% | 8.7% | 23.8% | 0.0% | 33.3% | 4 |
| 15 to 44 | 4.1% | 1.7% | 2.5% | 2.3% | 3.9% | 6 |
| 45 to 64 | 8.4% | 8.6% | 9.3% | 9.7% | 6.8% | 9 |
| 65 to 74 | 13.5% | 8.8% | 13.8% | 13.1% | 14.3% | 14 |
| 75 and over | 24.4% | 16.8% | 19.9% | 18.1% | 17.6% | 29 |
| Total | 12.4% | 9.1% | 11.3% | 10.0% | 9.8% | 74 |
Discussion
There continues to be a steep increase in scarlet fever notification and GP consultations early in the 2022 to 2023 season, with higher numbers than would be expected at this time of the year. The rate of iGAS infection notifications is following a similar pattern, with weekly incidence trending above what would be expected during the first part of the season, particularly in recent weeks.
While the rate of iGAS infection is elevated in all age groups, incidence in children aged under 10 years is high compared to levels reported in the last peak season preceding the COVID-19 pandemic – and substantially higher than the past 2 years. Investigations are underway following reports of an increase in lower respiratory tract GAS infections, particularly empyema, in children over the past few weeks. The current emm types have been circulating for the last 5 years, following the documented emergence and expansion of M1UK in 2016. Detailed genomic and biological investigations are underway to investigate any differences in the pathogen being seen this season.
The elevated iGAS levels in children compared to the period when pandemic control measures were in place is likely to be a consequence of the heightened scarlet fever activity given the crossover of strains associated in both presentations (1, 2).
Prompt treatment of scarlet fever with antibiotics is recommended to reduce risk of possible complications and limit onward transmission. Public health messaging to encourage contact with NHS 111 or GP practices for clinical assessment of patients with specific symptoms (for example, rash) has been issued along with reminders to provide ‘safety netting’ advice for parents indicating signs and symptoms of deterioration, particularly for children with respiratory viral infection. GPs and other frontline clinical staff are also reminded of the increased risk of invasive disease among household contacts of scarlet fever cases (3, 4).
At present the weekly rate of iGAS in individuals aged over 75 years is not exceeding pre-pandemic periods and the CFR is lower than previous years.
Clinicians should continue to be mindful of potential increases in invasive disease and maintain a high index of suspicion in relevant patients as early recognition and prompt initiation of specific and supportive therapy for patients with iGAS infection can be life-saving.
Relevant guidelines and information can be found on GOV.UK:
- Guidelines for the public health management of scarlet fever outbreaks in schools, nurseries and other childcare settings
- Scarlet fever: symptoms, diagnosis and treatment
- Guidelines for the management of close community contacts of invasive GAS cases and the prevention and control of GAS transmission in acute healthcare and maternity settings
- weekly notifiable diseases reports are published each week for a timelier update
- Group A Strep – what you need to know (blog post)
Invasive disease isolates and also non-invasive isolates from suspected clusters or outbreaks should be submitted to:
Staphylococcus and Streptococcus Reference Section
Antimicrobial Resistance and Healthcare Associated Infections (AMRHAI)
UK Health Security Agency
61 Colindale Avenue
London
NW9 5HT
Data sources and methods
Scarlet fever notification data was extracted from the notifications of infectious diseases (NOIDs) reports, data for England was extracted on 14 December 2022. iGAS laboratory notification data was extracted from the UK Health Security Agency Second Generation Surveillance System (SGSS) and combined with specimen referrals to the Staphylococcus and Streptococcus Reference Section to produce a total number of episodes for England. Data was extracted on 14 December 2022.
A season runs from week 37 to week 36 each year (mid-September to mid-September). The 2022 to 2023 season data within this report covers 12 September 2022 to 11 December 2022.
All-cause deaths within +/- 7 days: Reported date of death (obtained from tracing against the NHS SPINE where patient information is available) is compared to the date of iGAS specimen in a patient. Those where the difference between the 2 dates is ≤ plus 7 days and ≥ minus 7 days (to include those potentially diagnosed via post mortem). Follow-up was not possible for all reported iGAS cases, primarily due to poor identifier (NHS number and date of birth) completion. In addition, not all iGAS cases have the full 7-day follow-up period for case fatality assessment. CFR should be interpreted with caution given the small numbers involved.
Population rates are calculated per 100,000 using the relevant year ONS mid-year population estimate.
The M protein gene (emm) encodes the cell surface M virulence protein.
Prior to the COVID-19 pandemic, there were a number of seasons with elevated incidence of scarlet fever and iGAS, in particular, the 2017 to 2018 season. This has been used as a comparison point to the trends in the current season. During the pandemic there was an unprecedented reduction in the number of scarlet fever and iGAS notifications, affecting the 2019 to 2020 season, and the 2021 to 2022 season.
References
1. Chalker V, Jironkin A, Coelho J, Al-Shahib A, Platt S, Kapatai G, and others (2017). ‘Genome analysis following a national increase in scarlet fever in England 2014’. BMC Genomics: volume 18 number 1, page 224
2. Al-Shahib A, Underwood A, Afshar B, Turner CE, Lamagni T, Sriskandan S, and others (2106). Emergence of a novel lineage containing a prophage in emm/M3 group A Streptococcus associated with upsurge in invasive disease in the UK’. mGen; volume 2 number 11
3. Lamagni T, and others (2018). ‘Resurgence of scarlet fever in England, 2014–16: a population based surveillance study’. The Lancet Infectious Diseases: volume 18, number 2, pages 180 to 187
4. Watts V, and others (2019). ‘Increased risk for Invasive Group A Streptococcus disease for household contacts of scarlet fever cases, England, 2011–2016’. Emerging Infectious Diseases: volume 25, number 3, pages 529 to 537
Acknowledgements
These reports would not be possible without the weekly contributions from microbiology colleagues in laboratories across England, without whom there would be no surveillance data.
The support from colleagues within UKHSA, and the AMRHAI Reference Unit in particular, is valued in the preparation of the report.
Feedback and specific queries about this report are welcome via [email protected]
