Health Equity Assessment Tool (HEAT): what it is and how to use it
Updated 23 August 2024
The Health Equity Assessment Tool (HEAT) consists of a series of questions and prompts designed to help you systematically assess health inequalities related to your work programme and identify what you can do to help reduce inequalities. The purpose of the tool is to help you:
- consider the equity issues to be addressed for a population in the planning or preparatory stages of programme or service development
- consider the requirements of the Equality Act 2010
- demonstrate compliance with the public sector equality duty (PSED)
HEAT has similarities to other health equity assessment tools but is unique in providing a lighter yet systematic framework for assessing and driving action to reduce health inequalities across a variety of settings and contexts inside and outside of the health sector.
It provides an easy-to-follow template which can be applied flexibly to suit your work programme. Its specific prompts ensure consideration of multiple dimensions of health inequalities. This tool is an opportunity to understand how structural discrimination is operating in the environment in which we work and to identify what specific steps may be taken to address this discrimination as part of your work programme, project or policy.
HEAT was originally published as a full version and a simplified version. We are no longer publishing the simplified version, and have revised the full version to make it easier to use and improve accessibility.
Accessing the tool
The tool is published alongside this document at Health Equity Assessment Tool (HEAT).
It is a document that you can download and complete according to your requirements. It is designed to be universally useable - the tool includes topic-specific prompts to help you complete your assessment.
How it’s structured - and when to use it
The tool has 4 stages:
- Prepare.
- Assess.
- Refine and apply.
- Review.
It is designed to be completed at the start of a work plan, but can be used during any stage of a project or programme cycle, to help you consider its potential effects.
In practice, your assessment is likely to be iterative and the tool will help you continuously improve the contribution of your work to reducing health inequalities. HEAT presents a cyclical process and it is advised that the user completes each of the stages. The final stage focuses on evaluation, which will inform the next cycle.
What to consider when using the tool
Health inequalities are unjust differences in health and wellbeing between different groups of people (communities) which are systematic and avoidable. Health inequalities exist across a range of dimensions or characteristics, listed below.
Communities that experience inequalities and may be impacted by your work should be considered and engaged in the process. Their lived experiences should be valued and used to shape decision-making. The detrimental impact of low trust and confidence between affected communities and statutory services causes and exacerbates healthcare inequalities and overall health disparities. This can be reduced by implementing the recommendations from a HEAT assessment.
Tackling health inequalities at scale is likely to require support from senior leaders in your organisation or the system you work in. We therefore recommend that the use of the HEAT process includes a collaborative and community-focused approach which is sponsored by a senior leader.
Dimensions or characteristics to consider
There are several different dimensions or characteristics to consider when completing HEAT. These overlapping dimensions are demonstrated pictorially in Figure 1, below.
1. Protected characteristics
The protected characteristics outlined in the Equality Act 2010 are:
- age
- sex
- race
- religion or belief
- disability
- sexual orientation
- gender reassignment
- pregnancy and maternity
- marriage and civil partnership
2. Socio-economic status
This refers to the social standing of an individual or a group. It is often measured as a culmination of educational attainment, income and occupation.
3. Geographic deprivation
This refers to the inequalities experienced by people because of whey they live (for example an urban, rural or coastal setting) and their accessibility to services.
4. Vulnerable and inclusion health groups
Examples of vulnerable and inclusion health groups include people experiencing homelessness, people in prison and young people leaving care.
Figure 1: overlapping dimensions of health inequalities
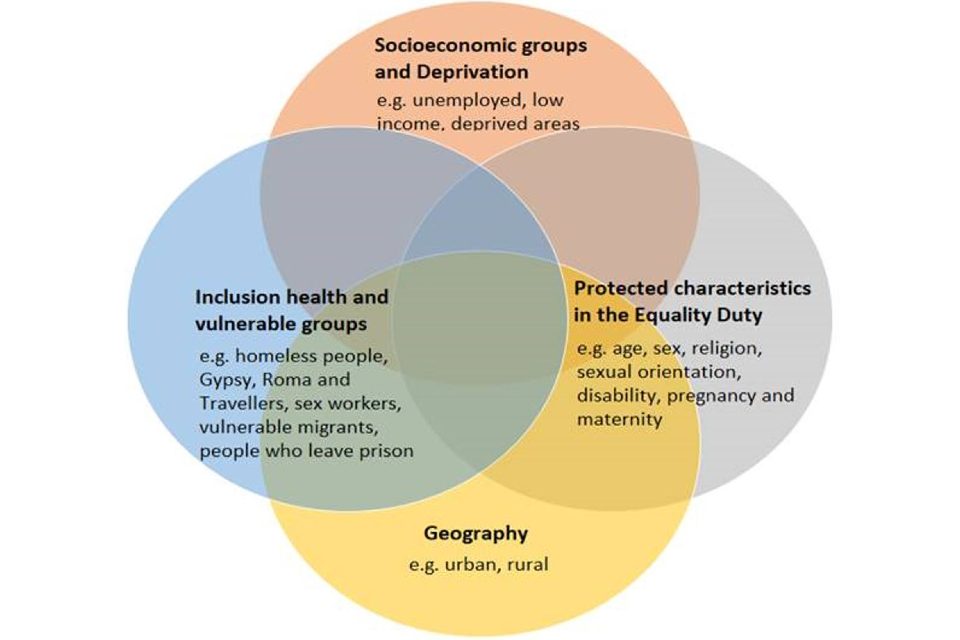
The tool recognises intersectionality - a concept for understanding how different aspects of a person’s identity (for example, gender, race, sexuality, religion, disability or age) combine to create different combinations of multiple discrimination - especially in particularly vulnerable groups - and privilege for others.
It also recognises the occurrence of multiple conditions and factors (such as physical health and mental health, or housing and mental health) that would require more integrated approaches to improve the quality of policy, programme or service design and delivery. This intersectionality is represented in Figure 1 by the overlap between dimensions.
Drivers of health inequalities
Health inequalities may be driven by:
- different experiences and distribution of the wider determinants of health or structural factors (for example, the environment, community life, income or housing) - in other words, the social, economic and environmental conditions in which people live, work and play
- different exposure to social, economic and environmental stressors and adversities, which affect states of mind from an early age and throughout life - stress and psychological wellbeing directly affect resilience, health conditions and health behaviours
- differences in health behaviours or other risk factors (including genetic vulnerability) which exist within and between groups - for example smoking, diet and physical activity levels have different social distributions. Health behaviours may be influenced by wider determinants of health, like income
- unequal access to or experience of health and other services between social groups
- inequalities impacted by structural discrimination which results in some groups and individuals - for example, those who identify with one or more of the protected characteristics - experiencing poorer access to services and poorer outcomes
Sustainability
Many equity projects and programmes are short-term pilots, some of which have proven inadequate for tackling long-term and pervasive inequalities. You should be assessing your plans for the medium to long-term sustainability of the piece of work and considering what will happen when the work ends. It is important to identify your senior sponsor from the outset who will champion the assessment’s findings and implementation.
Information and research
When completing HEAT, you will need to use evidence to support your responses. This includes data and expertise on health inequalities and successfulness of interventions. In some cases, this data may be limited and you may need to commission new research or engage with partners to obtain information, including local authorities, the Office for Health Improvement and Disparities (OHID) and NHS England.
If gathering additional data is not possible, you may need to notify decision-makers about the need for such data. Without good data, HEAT should be used cautiously, ensuring that the effects of your work on particularly vulnerable groups are not overlooked.
The tool includes links to some key data sources.
Additional resources
When completing HEAT, the following resources may be useful.
On GOV.UK:
- Health equity audit guide for screening providers and commissioners
- Local action on health inequalities: evidence papers
- Health disparities and health inequalities: applying All Our Health
- Public sector equality duty: guidance for public authorities
- A summary guide to the Equality Act 2010 for public sector organisations
- the Public Health Outcomes Framework
- A guide to community-centred approaches for health and wellbeing
From NHS England:
- HEAT e-learning module
- Equality and health inequality legal duties
- links to resources on inclusion health for people working in the health and care sector
- The Healthcare Inequalities Improvement Dashboard
- Core20PLUS5 (adults) – an approach to reducing healthcare inequalities
- Core20PLUS5 – an approach to reducing health inequalities for children and young people
It may be useful to tie your completion of HEAT into a sector-led improvement programme in your area, for example, the Local Government Association’s Sector-led improvement in public health.
Enquiries
If you have any enquiries about this guidance or the tool, you can contact us at [email protected].
