Prenatal pertussis vaccination coverage in England from October to December 2023
Updated 20 December 2024
Applies to England
Main points
This quarterly report evaluates prenatal pertussis vaccine coverage for women who delivered in the October to December 2023 quarter who were eligible for the prenatal pertussis vaccine from 16 weeks of pregnancy onwards. The main findings were that:
-
pertussis vaccine coverage in pregnant women for the third quarter of the 2023/24 financial year was 58.9% in October, 59.4% in November and 59.5% in December
-
the mean coverage for the quarter was 59.3%, which was 2.1% lower than the mean coverage for the same quarter in the 2022/23 financial year
-
at sub-national level, the South East commissioning region had the highest mean coverage with 66.1% while the London commissioning region had the lowest with 36.8%
-
there was a 15.7% decline in coverage compared to the peak coverage in the same reporting quarter of 2016/17
-
this observed decline in coverage has largely been driven by a decrease in London NHS commissioning region but is also reflected in other regions, such as the North West and the Midlands
Introduction
This report presents pertussis vaccine coverage in pregnant women in England for the period October to December 2023, updating previous data reported for July to September 2023 (1).
Following increased pertussis activity in all age groups, including infants under 3 months of age, and the declaration of a national pertussis outbreak in April 2012 (2), the pertussis vaccine has been offered to pregnant women since 1 October 2012 (3). The prenatal pertussis vaccination programme aims to minimise disease, hospitalisation and deaths in young infants, through the intra-uterine transfer of maternal antibodies, until they can be actively protected by the routine infant programme with the first dose of pertussis vaccine scheduled at 8 weeks of age (4).
In June 2014, the Joint Committee on Vaccination and Immunisation (JCVI) advised it should continue for a further 5 years (5). In February 2016, the JCVI considered new evidence demonstrating that vaccination earlier in pregnancy would increase opportunities during pregnancy for vaccination, without detrimentally affecting the protection afforded to the infant (6, 7). Based on this, JCVI advised that vaccination could be offered from gestational week 16, although for operational reasons vaccination should ideally be offered from around 20 weeks, on or after the foetal anomaly scan (8).
This advice was implemented from April 2016 as was offering the vaccine through general practice as well as some maternity services. In 2019, following the JCVI recommendation, the prenatal pertussis vaccine became a routine programme in England (9).
In response to the coronavirus (COVID-19) pandemic, nationwide social distancing measures were initiated from 23 March 2020. To minimise disruptions, guidance to continue routine vaccination programmes with priority given to time sensitive vaccines, such as prenatal pertussis vaccines, were outlined by NHS England at the beginning of the pandemic (10).
In addition, the Royal College of Nursing published guidance on the management of immunisation clinics, and the then Public Health England (PHE) produced resources promoting immunisations to pregnant women and young families (11, 12).
Methods
General practice (GP) level pertussis vaccine coverage data is automatically uploaded via participating GP IT suppliers to the ImmForm website each month. ImmForm data is validated and analysed by the UK Health Security Agency (UKHSA) to check data completeness, identify and query any anomalous data and describe epidemiological trends. Since April and May 2016 (implementation date varied by GP IT supplier), the following monthly data has been collected:
- denominator: number of women who delivered in the survey month, excluding miscarriages and stillbirths, regardless of gestational age
- numerator: number of women receiving pertussis vaccination between week 16 of pregnancy and delivery
For accurate denominators to be extracted from GP IT systems by the automated survey and precise coverage estimates to be calculated, it is important that the medical records of all women who have given birth have the following fields completed:
- the date of delivery
- the date of receipt of a pertussis-containing vaccine at or after week 16 of pregnancy, regardless of the setting where the vaccine was administered
- where relevant, fields indicating stillbirth or miscarriage
Coverage by former local teams and NHS commissioning regions (based on the 2019 NHS England configurations) is also included, for comparison, in the data tables associated with this report.
Participation and data quality
All GP IT suppliers provided data for the October to December 2023 period. National GP practice participation was at 98.7% in October, 98.5% in November and 98.5% in December.
Results
Monthly pertussis vaccine coverage across the quarter showed that 58.9% in October, 59.4% in November and 59.5% in December, with mean coverage for the quarter at 59.3% (Table 1, Figure 1, and see data tables associated with this report). During this quarter, prenatal pertussis vaccine coverage by ICB ranged from 81.1% (Derby and Derbyshire, October 2023) to 24.5% (North Central London, November 2023) (Table 1).
When comparing change in percentage coverage from the 2022 to 2023 financial year, national coverage was 2.8% lower in October, 1.8% lower in November and 1.9% lower in December. Mean coverage for this quarter was 2.1% lower than national coverage reported for the same quarter in the 2022/23 financial year (13).
Coverage by former local teams and NHS commissioning regions (based on the 2019 NHS England configurations) are also included in the data tables associated with this report, for trend comparisons.
In the London NHS commissioning region there has been a steep decline in coverage since June 2019. Coverage in London decreased to its lowest in October 2023, at 36.3%, a fall of 24.6 percentage points from the peak in December 2019, when coverage was 60.9% (Figure 2). Coverage in the North West region increased in the reporting period, with an increase of 7.8 percentage points between June 2023 to November 2023.
Table 1. Monthly pertussis vaccination coverage (%) in pregnant women by ICB in England, January to March 2024
| ICB code | ICB name | January 2024 | February 2024 | March 2024 | January to March 2024 |
|---|---|---|---|---|---|
| QE1 | Lancashire and South Cumbria | 57.1 | 62.3 | === | 60.4 |
| QF7 | South Yorkshire | 64.7 | 66.8 | === | 66.3 |
| QGH | Herefordshire and Worcestershire | 65.9 | 61.4 | === | 66.3 |
| QH8 | Mid and South Essex | 65.1 | 61.6 | === | 64.4 |
| QHG | Bedfordshire, Luton and Milton Keynes | 59.3 | 63.4 | === | 62.2 |
| QHL | Birmingham and Solihull | 44.1 | 46.8 | === | 49.5 |
| QHM | North East and North Cumbria | 63.2 | 64.3 | === | 64.8 |
| QJ2 | Derby and Derbyshire | 81.1 | 80.3 | === | 80.1 |
| QJG | Suffolk and North East Essex | 64 | 63.2 | === | 66.6 |
| QJK | Devon | 67.3 | 69.4 | === | 68.1 |
| QJM | Lincolnshire | 61.1 | 61.5 | === | 64 |
| QK1 | Leicester, Leicestershire and Rutland | 56.3 | 57.3 | === | 62 |
| QKK | South East London | 49.8 | 52.3 | === | 50 |
| QKS | Kent and Medway | 65.2 | 64.6 | === | 64.3 |
| QM7 | Hertfordshire and West Essex | 66.5 | 64.8 | === | 65.4 |
| QMF | North East London | 29.9 | 28.8 | === | 29.9 |
| QMJ | North Central London | 25.9 | 24.5 | === | 25 |
| QMM | Norfolk and Waveney | 78.5 | 73.5 | === | 75 |
| QNC | Staffordshire and Stoke-on-Trent | 62.5 | 63.1 | === | 65.7 |
| QNQ | Frimley | 58 | 59.1 | === | 62.3 |
| QNX | Sussex | 65.7 | 58.1 | === | 57 |
| QOC | Shropshire, Telford and Wrekin | 73.8 | 74.1 | === | 75.3 |
| QOP | Greater Manchester | 51.7 | 54.5 | === | 53.5 |
| QOQ | Humber and North Yorkshire | 72.8 | 73.1 | === | 73.4 |
| QOX | Bath and North East Somerset, Swindon and Wiltshire | 50.1 | 47.1 | 52.4 | |
| QPM | Northamptonshire | 48.7 | 53.8 | === | 55.3 |
| QR1 | Gloucestershire | 64.5 | 64.9 | === | 65.8 |
| QRL | Hampshire and Isle of Wight | 70.6 | 72.1 | === | 69.4 |
| QRV | North West London | 32.5 | 35.2 | === | 34.5 |
| QSL | Somerset | 57.2 | 66.4 | === | 61.6 |
| QT1 | Nottingham and Nottinghamshire | 64.6 | 68 | === | 69.4 |
| QT6 | Cornwall and The Isles of Scilly | 58.4 | 63.2 | === | 54.2 |
| QU9 | Buckinghamshire, Oxfordshire and Berkshire West | 68.8 | 70.6 | === | 68.2 |
| QUA | Black Country | 56.1 | 57.8 | === | 59.7 |
| QUE | Cambridgeshire and Peterborough | 65.2 | 65.9 | === | 65.5 |
| QUY | Bristol, North Somerset and South Gloucestershire | 69.9 | 69.2 | === | 67.8 |
| QVV | Dorset | 69.2 | 71.8 | === | 72.5 |
| QWE | South West London | 46.5 | 47.5 | === | 46.5 |
| QWO | West Yorkshire | 67.2 | 67.6 | === | 67.6 |
| QWU | Coventry and Warwickshire | 62.1 | 55.5 | === | 58.7 |
| QXU | Surrey Heartlands | 70.1 | 70.8 | === | 71.9 |
| QYG | Cheshire and Merseyside | 64.9 | 65 | === | 63.4 |
| Total | – | 58.9 | 58.9 | 58.9 | 59.4 |
Figure 1. Monthly pertussis vaccination coverage (%) in pregnant women (England), 2016 to 2023
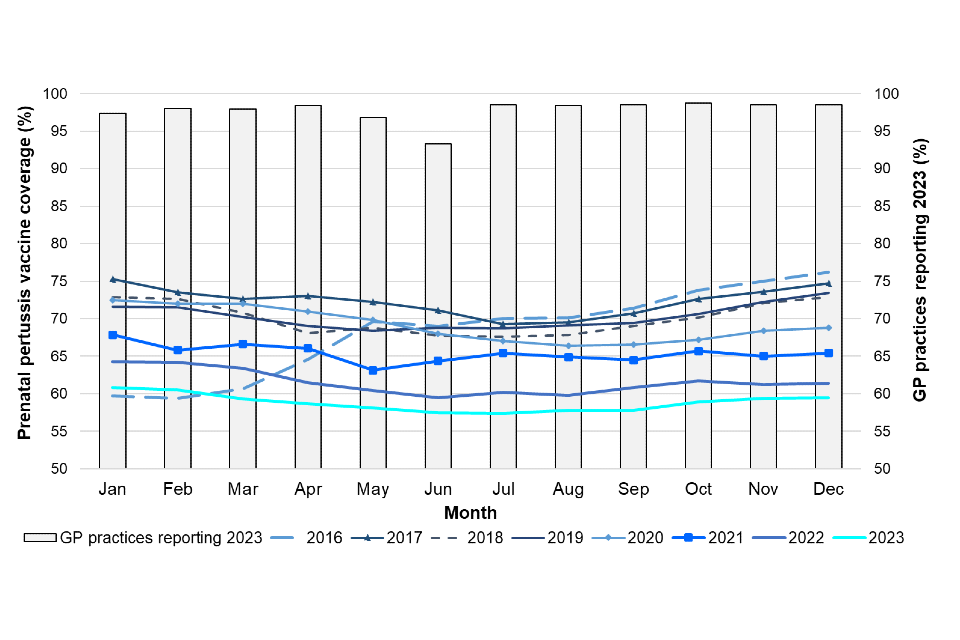
Figure 2. Monthly pertussis vaccination coverage (%) in pregnant women by NHS commissioning region, April 2019 to December 2023 [Note 1]

Note 1: Data from the smallest IT supplier was excluded between November to December 2019.
Discussion
This third quarterly report of 2023/24 evaluates pertussis vaccine coverage for women who delivered in the October to December 2023 quarter.
Overall, monthly prenatal pertussis vaccine coverage in the third reporting quarter of 2023/24 went from 58.9% in October, to 59.4% in November and to 59.5% in December. From October to December 2023, the difference in mean coverage between the highest and the lowest performing ICBs was 55.4%.
Coverage in the London NHS commissioning region has continuously been considerably lower than all other regions, with coverage 30.3% lower than the region with the highest coverage (North East and Yorkshire) in this reporting quarter.
Limitations to the data presented in this report may explain some of the observed variability in coverage at the local level and over time. First, completeness of data is reliant on the recording of delivery dates in the mother’s medical records and a recent study in England suggests that maternity notes regarding pregnancy and delivery are often scanned or archived, rather than coded in an extractable format (15). Furthermore, a comparison of this denominator data with national data on live births (16) indicates that, in 2022, this data represented about 73% of the population of pregnant women.
Continued support in the delivery of this important programme has been sought from service providers (GP practices and maternity units). Screening and Immunisation Teams and HPTs should continue to update service providers on the current epidemiology of the disease and the need to maintain and improve coverage achieved thus far.
If coverage, and ultimately the impact of the programme itself, is to be accurately monitored, it is essential that GPs and practice nurses continue to ensure that vaccination and date of delivery are recorded in the patient’s GP record.
In areas that have commissioned maternity units to offer pertussis vaccines in pregnancy, it is important that providers ensure doses of vaccines given to individual women are also communicated to the woman’s GP. Maternity units not offering pertussis vaccines to pregnant women should continue to discuss its importance, make use of available resources on GOV.UK, and signpost women to their GP to receive the vaccine.
GPs, practice nurses, obstetricians and midwives should continue to encourage pregnant women to receive the pertussis vaccine – ideally between weeks 20 and 32 of their pregnancy (but up to term) – so as to optimise protection for their babies from birth (8).
References
1. UKHSA (2023). Prenatal pertussis vaccination coverage in England from January to March 2023 and annual coverage for 2022 to 2023. Health Protection Report: volume 17, number 10
2. A level 3 incident is the third of 5 levels of alert under the PHE’s incident Reporting and information System (IERP) according to which public health threats are classified and information flow to the relevant outbreak control team is coordinated. A level 3 incident is defined as one where the public health impact is significant across regional boundaries or nationally. An IERP level 3 incident was declared in April 2012 in response to the ongoing increased pertussis activity
3. DHSC (2012). Pregnant women to be offered whooping cough vaccination
4. UKHSA (2023). ‘Complete routine immunisation schedule’
5. JCVI (2014). Minute of the meeting on 4 June 2014
6. Eberhardt CS, Blanchard-Rohner G, Lemaitre B, Boukrid M, Combescure C, Othenin-Girard V and others (2016). ‘Maternal immunization earlier in pregnancy maximizes antibody transfer and expected infant seropositivity against pertussis’. Clinical Infectious Diseases: volume 62, pages 829 to 836
7. JCVI (2016). Minute of the meeting on 3 February 2016
8. PHE (2016). The Green Book, chapter 24: Pertussis
9. JCVI (2019). Minute of the meeting on 5 June 2019
10. NHS England (2020). Preparedness letter for general practice
11. Royal College of Nursing (2020) Immunisation
12. PHE (2020) Vaccine update: World Immunisation Week
13. PHE (2016) Pertussis Vaccination Programme for Pregnant Women: vaccine coverage estimates in England, October to December 2016
14. Llamas A, Amirthalingam G, Andrews N, and Edelstein M (2020). ‘Delivering prenatal pertussis vaccine through maternity services in England: what is the impact on vaccine coverage?’ Vaccine: volume 38, issue 33, pages 5,332 to 5,336
15. Office for National Statistics (2022). Births in England and Wales
16. PHE (2017). Pregnancy: How to help protect yourself and your baby
