Spotlight on sexually transmitted infections in the North West: 2021 data
Updated 5 March 2024
Applies to England
Summary
Sexually transmitted infections (STIs) represent an important public health problem in the North West. Out of all the UK Health Security Agency (UKHSA)’s regions, it had the second highest rate of new STIs in England.
A total of 35,436 new STIs were diagnosed in North West residents in 2021, representing a rate of 481 diagnoses per 100,000 population. Rates by upper tier local authority ranged from 176 new STI diagnoses per 100,000 population in Sefton to 936 new STI diagnoses per 100,000 population in Liverpool. The number of new STIs diagnosed in North West residents increased by 6% between 2020 and 2021.
Increases in diagnosis of the 5 major STIs were seen in:
- syphilis (15%)
- gonorrhoea (15%)
- chlamydia (8%)
- genital herpes (1%)
Genital warts decreased by 6%.
In June 2021, the National Chlamydia Screening Programme (NCSP) changed to focus on reducing reproductive harm of untreated infection in young women. This led to a change in the recommended chlamydia detection rate indicator (DRI) included in the Public Health Outcomes Framework (PHOF).
UKHSA recommends that local authorities work towards the revised female-only PHOF benchmark DRI of 3,250 per 100,000 females aged 15 to 24 years. This report relates to 2021 data, for the most part of which the NCSP recommended an offer of screening to all sexually active young people aged under 25 years.
In 2021, the chlamydia diagnosis rate among North West residents aged 15 to 24 years (all recorded genders) was 1,330 per 100,000 residents, against the previous recommended DRI of least 2,300 per 100,000 residents aged 15 to 24 years (all recorded genders).
Where gender and sexual orientation are known, gay, bisexual and other men who have sex with men (GBMSM) account for 22% of North West residents diagnosed with a new STI, excluding chlamydia diagnoses reported via the Chlamydia Testing Activity Dataset (CTAD) surveillance system (78% of those diagnosed with syphilis and 44% of those diagnosed with gonorrhoea).
STIs disproportionately affect young people. North West residents aged between 15 and 24 years accounted for 48% of all new STI diagnoses in 2021. A steep decline (94% decrease) has been seen between 2017 and 2021 in genital warts diagnosis rates in females aged 15 to 19 years. This follows the introduction in 2008 of vaccination against human papillomavirus (HPV), the virus that causes genital warts, for females aged 12 to 13 years.
The white ethnic group has the highest number of new STI diagnoses (24,471, 86%). Although only 1% of new STIs are in the black Caribbean ethnic group, it has the highest rate (1,820 per 100,000), which is 5 times the rate seen in the white ethnic group. Where country of birth was known, 89% of North West residents diagnosed with a new STI in 2021 (excluding chlamydia diagnoses reported via CTAD) were UK-born.
Conclusions
Following the disruptions in service delivery during the first year of the coronavirus (COVID-19) pandemic, the number of consultations at sexual health services (SHSs) increased between 2020 and 2021 and now exceeds the number reported in 2019. This provides evidence of a recovery in service provision, after the lifting of COVID-19 restrictions in the summer of 2021, partially driven by the continued widespread provision of online consultations.
The number of sexual health screens (for chlamydia, gonorrhoea, syphilis and HIV) in England also increased between 2020 and 2021, although the number of STI diagnoses remained stable. The increase in sexual health screens may be a result of built-up demand for SHSs as well as a return to pre-COVID-19 pandemic levels of social and sexual mixing and the substantial number of tests being accessed through online services (1 to 4).
It will remain important to continue to monitor and understand whether these changes have affected equity of access to SHSs (5, 6).
Chlamydia continues to account for the majority of STI diagnoses made in 2021, a large proportion of which are related to the NCSP. Screening rates for chlamydia have recovered gradually since the pandemic, with an increasing proportion of tests and diagnoses being made via internet services.
Although overall STI diagnoses rates remained similar between 2020 and 2021, there was an increase in bacterial STI diagnoses among GBMSM.
STIs continue to show geographic and socioeconomic variation and disproportionately impact GBMSM, people of black Caribbean ethnicity, and young people aged 15 to 24 years.
UKHSA’s main messages
Providers and commissioners have an important role in communicating messages about safer sexual behaviours and how to access services.
Important prevention messages
Using condoms consistently and correctly protects against HIV and other STIs such as chlamydia, gonorrhoea and syphilis and can prevent unplanned pregnancy.
Regular screening for STIs and HIV is essential to maintain good sexual health. Everyone should have an STI screen, including an HIV test, on at least an annual basis, if having condomless sex with new or casual partners.
In addition:
- women and other people with a womb or ovaries under the age of 25 years who are sexually active should have a chlamydia test annually and on any change of sexual partner
- GBMSM should have an annual test for HIV and STIs or every 3 months, if having condomless sex with new or casual partners
HIV pre-exposure prophylaxis (PrEP) can also be used to provide protection to people at risk of HIV while HIV post-exposure prophylaxis (PEP) can be used after condomless sex if someone has potentially been exposed to HIV, to reduce the risk of contracting HIV. Both of these can be obtained from specialist SHSs.
People living with diagnosed HIV who are on treatment and have an undetectable viral load are unable to pass on the infection to others during sex. This is known as ‘Undetectable = Untransmittable’ or ‘U=U’.
Vaccination against mpox (monkeypox) virus, HPV, hepatitis A and hepatitis B will protect against disease caused by these viruses and prevent the spread of these infections:
- GBMSM can obtain the mpox, hepatitis A and hepatitis B vaccines from specialist SHSs; these vaccines are also available for other people at high risk of exposure to the viruses
- GBMSM aged 45 years and under, can also obtain the HPV vaccine from specialist SHSs
SHSs are free and confidential and offer testing and treatment for HIV and STIs, condoms, vaccination, HIV PrEP, and PEP:
- online self-sampling for HIV and STIs is widely available
- information and advice about sexual health, including how to access services, is available at Sexwise and from the national sexual health helpline on 0300 123 7123
Charts, tables and maps
Figure 1. New STI diagnosis rates by UKHSA region of residence, England, 2021
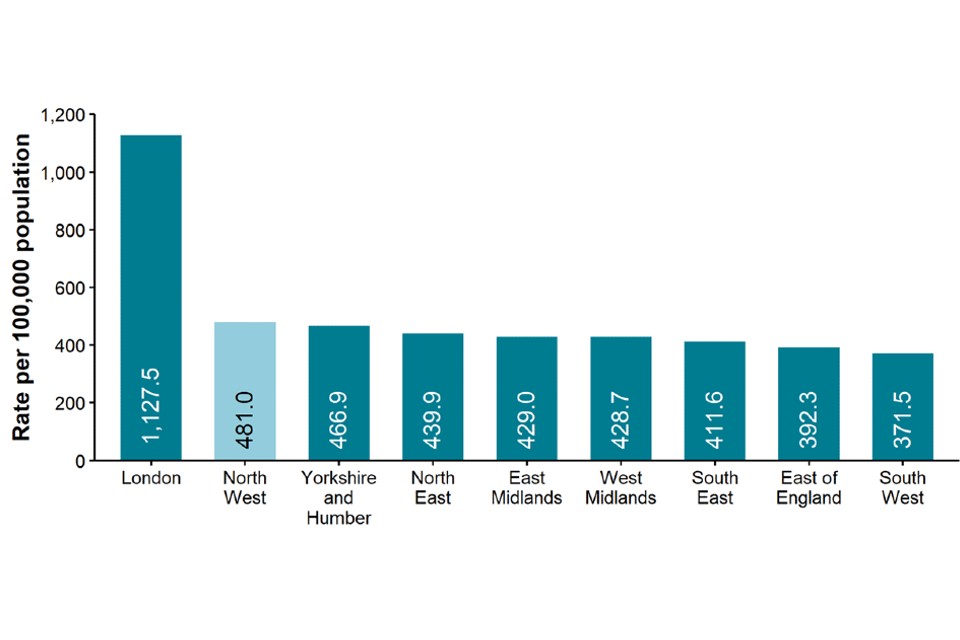
Data sources: GUMCAD STI surveillance system (GUMCAD), CTAD
Figure 1 is a bar chart showing that the rate of new STI diagnoses per 100,000 in the North West (481.0) was the second highest in the country, with London having the highest rate (1,127.5).
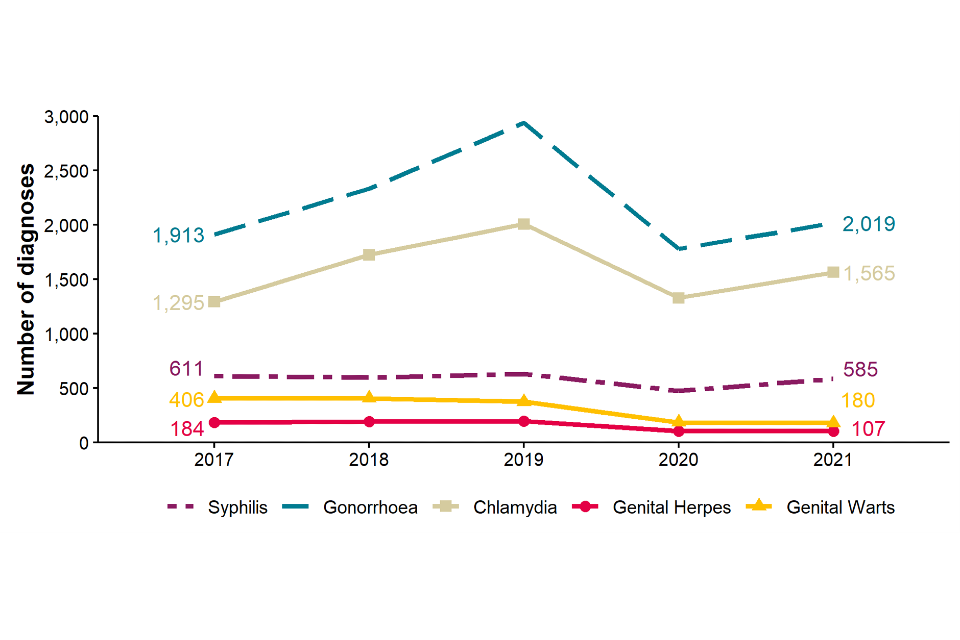
Figure 2. Number of diagnoses of the 5 main STIs, North West residents, 2017 to 2021
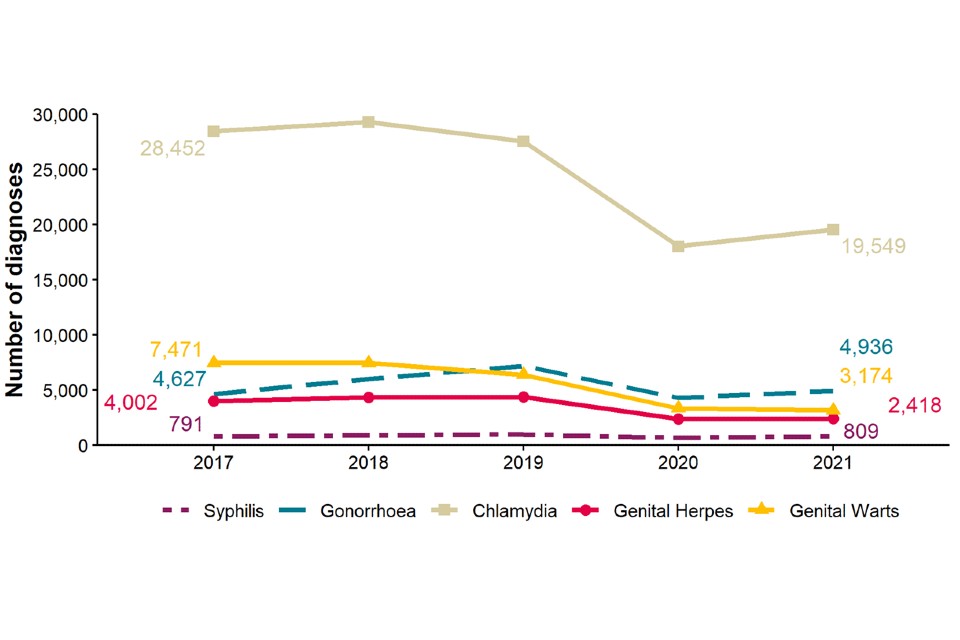
Data sources: GUMCAD, CTAD
[note 1] Any increase in gonorrhoea diagnoses may be due to the increased use of highly sensitive nucleic acid amplification tests (NAATs) and additional screening of extra-genital sites in GBMSM. Any decrease in genital wart diagnoses may be due to a moderately protective effect of HPV-16/18 vaccination. Any increase in genital herpes diagnoses may be due to the use of more sensitive NAATs. Increases or decreases may also reflect changes in testing practices
Figure 2 shows trend lines of the number of diagnoses of the 5 main STIs for North West residents. It shows a slight increase in chlamydia from 2020 to 2021, and similar trends for syphilis and gonorrhoea. Genital herpes and genital warts have stayed roughly the same from 2020 to 2021.
Figure 3. Diagnosis rates of the 5 main STIs, North West residents, 2017 to 2021
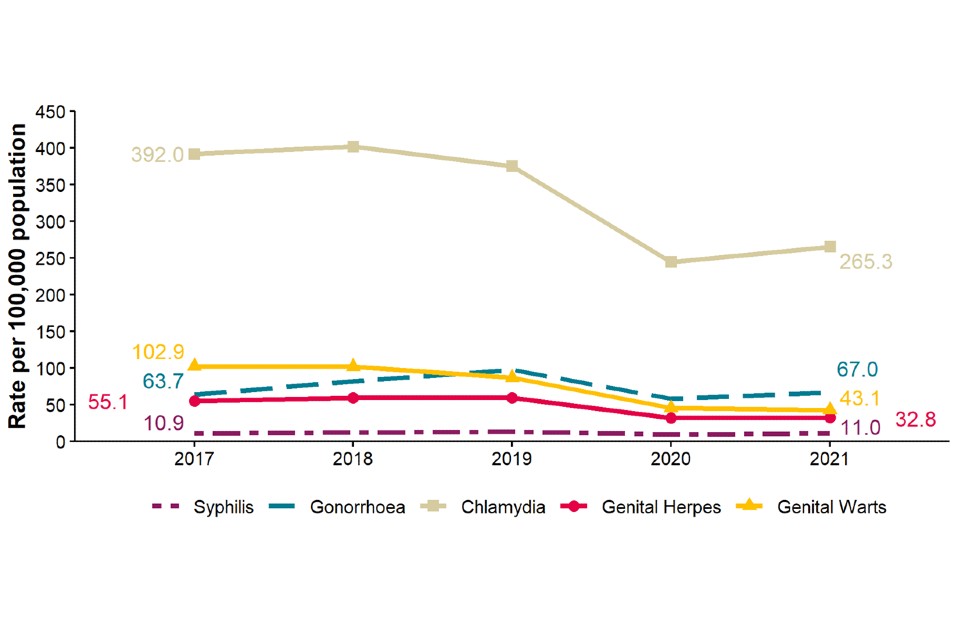
Data sources: GUMCAD, CTAD
See [note 1] above.
Figure 3 shows a trend line of the diagnosis rates of the 5 main STIs among North West residents, which shows the same trends as Figure 2.
Table 1. Percentage change in new STI diagnoses, North West residents
| Diagnoses | 2021 | Percentage change 2017 to 2021 | Percentage change 2020 to 2021 |
|---|---|---|---|
| New STIs | 35,436 | -33% | 6% |
| Syphilis | 809 | 2% | 15% |
| Gonorrhoea | 4,936 | 7% | 15% |
| Chlamydia | 19,549 | -31% | 8% |
| Genital herpes | 2,418 | -40% | 1% |
| Genital warts | 3,174 | -58% | -6% |
Data sources: GUMCAD, CTAD
See [note 1] above.
Table 1 shows that chlamydia was the most commonly diagnosed STI with 19,549 diagnoses in 2021. The greatest proportional increases from 2017 to 2021 were seen in syphilis and gonorrhoea diagnoses, increasing by 2% and 7% respectively. The greatest proportional fall from 2017 to 2021 was in genital warts (by 58%).
Figure 4. Rates of new STIs per 100,000 residents by age group (for those aged 15 to 64 years only) and gender in the North West, 2021
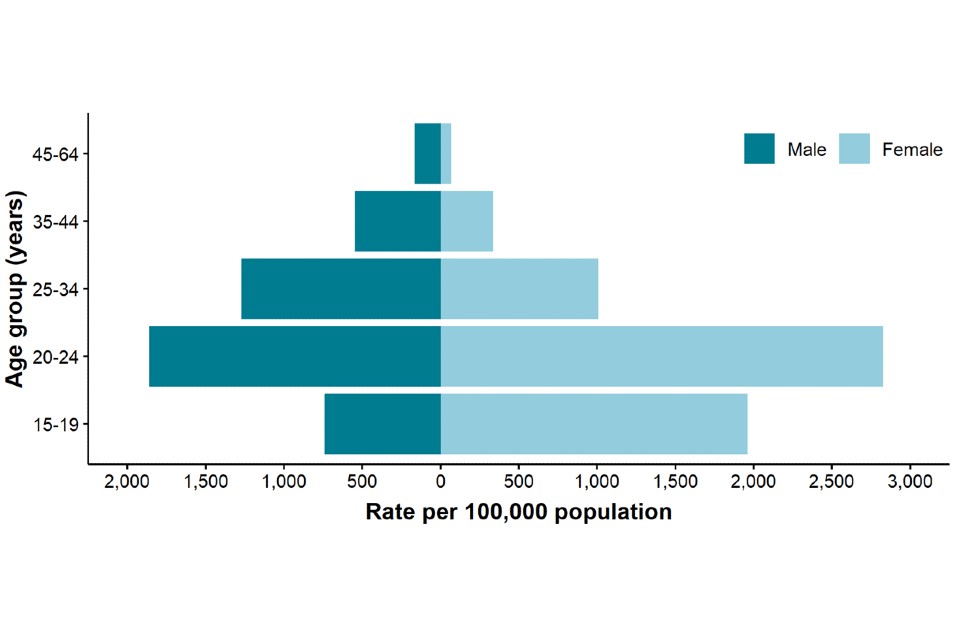
Data sources: GUMCAD, CTAD
Figure 4 is a bar chart showing rates of STIs by age group. The highest rates are seen in females aged 20 to 24 years.
Figure 5. Rates of gonorrhoea per 100,000 residents by age group [note 2] in the North West, 2017 to 2021
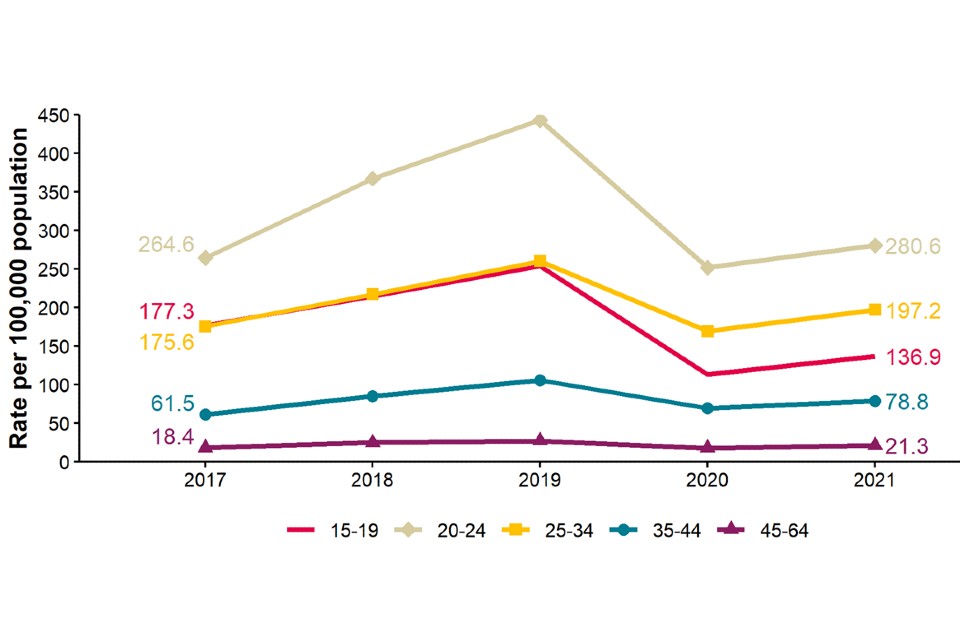
Data source: GUMCAD
[note 2] Age-specific rates are shown for those aged 15 to 64 years only.
Figure 5 shows rates of gonorrhoea per 100,000 residents by age group in the North West, for 2017 to 2021. Rates were highest in those aged 20 to 24 years. Rates in all age groups declined from 2019 to 2020 but slightly increased from 2020 to 2021 again.
Figure 6. Rates of genital warts per 100,000 residents aged 15 to 19 years by gender in the North West, 2017 to 2021
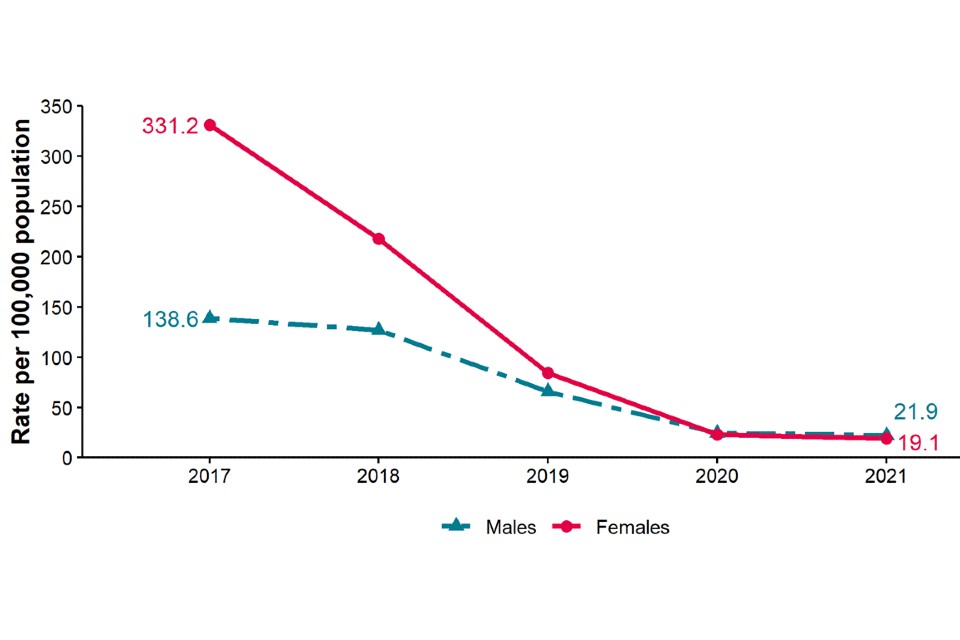
Data source: GUMCAD
Figure 6 shows rates of genital warts per 100,000 residents aged 15 to 19 years by gender in the North West. It shows that rates in both males and females fell from 2017 to 2021, with the rate of decrease being higher among females.
Figure 7. Rates of new STIs by ethnic group per 100,000 residents in the North West, 2021
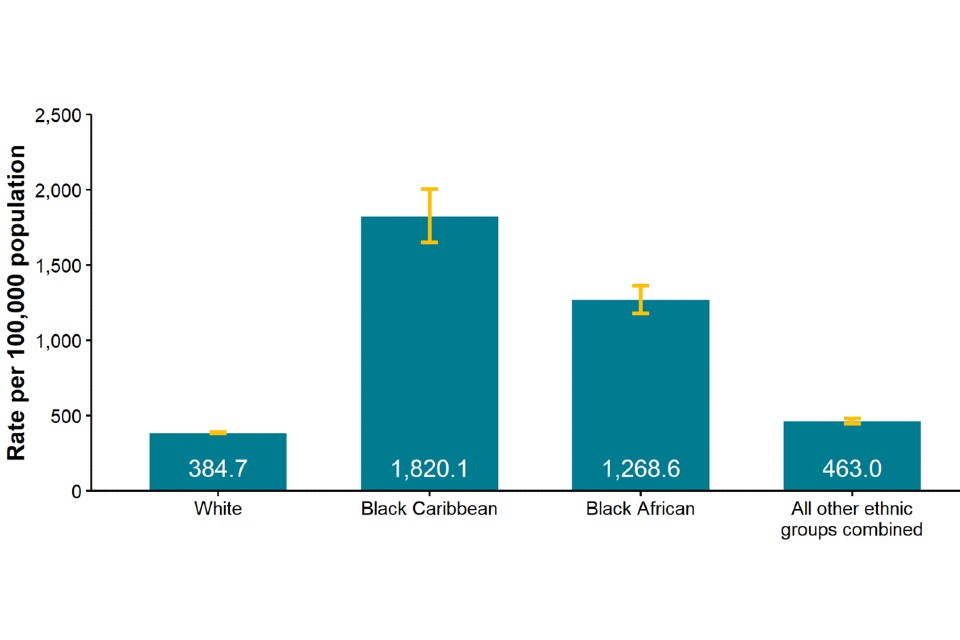
Data sources: GUMCAD, CTAD
Figure 7 is a bar chart showing rates by ethnicity per 100,000 population of North West residents diagnosed with a new STI in 2021. It shows that rates in the black Caribbean ethnic group per 100,000 were significantly higher than rates in white and black African and other ethnic groups.
Table 2. Proportion of North West residents diagnosed with a new STI by ethnicity, 2021
| Ethnic group | Number | Percentage excluding unknown |
|---|---|---|
| White | 24,471 | 86% |
| Black Caribbean | 421 | 1% |
| Black African | 752 | 3% |
| All other ethnic groups combined | 2,815 | 10% |
| Unknown | 6,977 |
Data sources: GUMCAD, CTAD
Table 2 shows that the highest numbers of STIs were in white (24,471) population groups, representing 86% of the total. Black Caribbean population groups made up 1%, black African 3% and other black and minority ethnic groups 10% of the total where ethnicity was known.
Figure 8. Proportion of North West residents diagnosed with a new STI by world region of birth [note 3], 2021
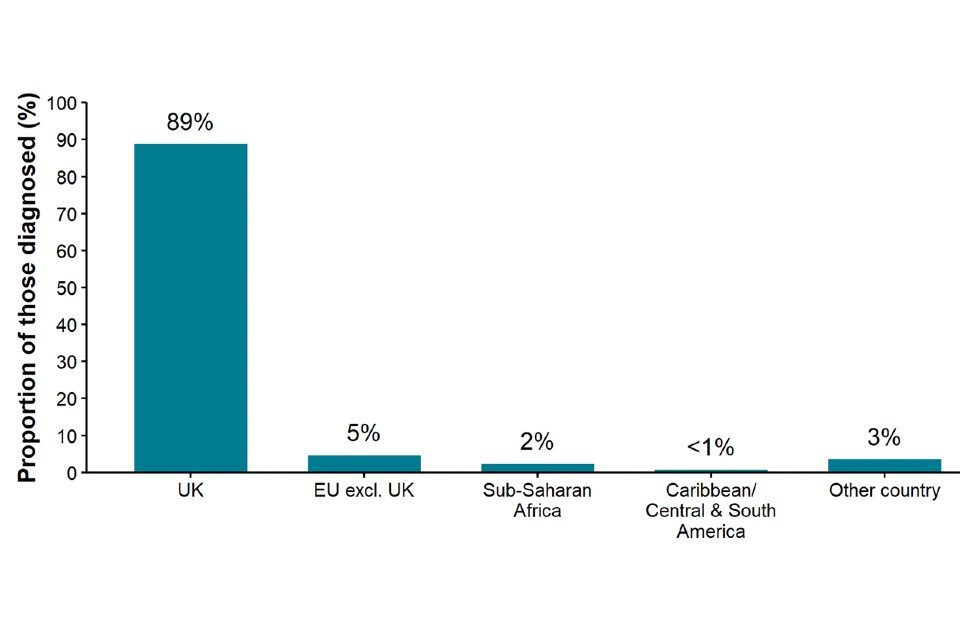
Data source: GUMCAD
[note 3] Data on country of birth is not collected by CTAD. All information about world region of birth is based on diagnoses made in specialist and non-specialist services that report to GUMCAD.
Figure 8 is a bar chart showing the proportion of North West residents diagnosed with a new STI by world region of birth in 2021. It shows that UK-born constitute the highest proportion of North West residents diagnosed with a new STI (89%), with the next highest being EU-born (5%).
Figure 9. Diagnoses of the 5 main STIs among GBMSM [note 4], North West residents, 2017 to 2021
Data source: GUMCAD
[note 4] Data on sexual orientation is not collected by CTAD. All information about GBMSM is based on diagnoses made in specialist and non-specialist services which report to GUMCAD.
GUMCAD started in 2009. Reporting of sexual orientation is less likely to be complete for earlier years, so rises seen may be partly artefactual.
Any increase in gonorrhoea diagnoses may be due to the increased use of highly sensitive nucleic acid amplification tests and additional screening of extra-genital sites in GBMSM. Any decrease in genital wart diagnoses may be due to a moderately protective effect of HPV-16/18 vaccination. Any increase in genital herpes diagnoses may be due to the use of more sensitive NAATs. Any increase or decrease may reflect changes in testing.
Figure 9 shows trend lines for diagnoses of the 5 main STIs in specialist sexual health clinics (SHCs) among GBMSM North West residents, from 2017 to 2021. It shows increases in the number of diagnoses of gonorrhoea, chlamydia, and syphilis from 2017 to 2019, with a subsequent fall from 2019 to 2020, and a slight increase from 2020 to 2021. The number of genital herpes and genital warts diagnoses fell from 2017 to 2021.
Table 3. Percentage change in new STI diagnoses in GBMSM* residents in the North West
| Diagnoses | 2021 | Percentage change 2017 to 2021 | Percentage change 2020 to 2021 |
|---|---|---|---|
| New STIs | 4,963 | -9% | 14% |
| Syphilis | 585 | -4% | 23% |
| Gonorrhoea | 2,019 | 6% | 13% |
| Chlamydia | 1,914 | 48% | 28% |
| Genital herpes | 107 | -42% | -1% |
| Genital warts | 180 | -56% | -4% |
Data source: GUMCAD
See [note 4] above.
Table 3 shows the number of the main STI diagnoses among GBMSM that were resident in the North West in 2021 and the percentage change since 2017 and 2020. It shows that gonorrhoea was the most common STI in GBMSM in 2021.
From 2017 to 2021, a large proportional increase was seen in chlamydia (48%) and increases were also seen in gonorrhoea (6%). The number of syphilis, genital herpes, and genital warts diagnoses fell from 2017 to 2021. The total number of STIs decreased from 2017 to 2021 by 9%.
Figure 10a. Rate of new STI diagnoses per 100,000 population among North West residents by upper tier local authority of residence, 2021
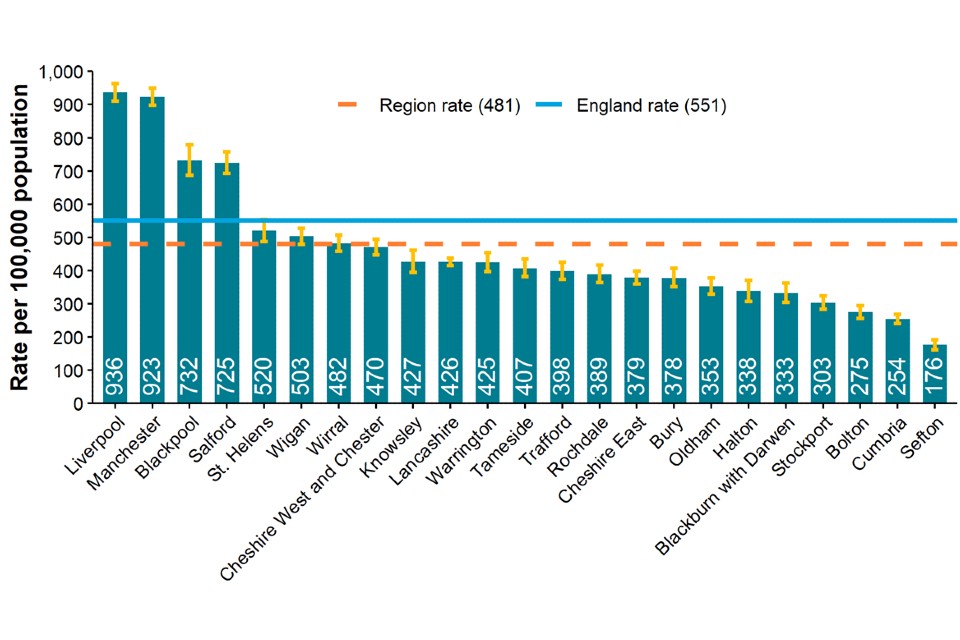
Data sources: GUMCAD, CTAD
Figure 10a is a bar chart showing the rate of new STI diagnoses per 100,000 population among North West residents by local authority of residence in 2021, compared to the regional (481) and national (551) rate. The rates per 100,000 in local authorities ranged from 176 in Sefton to 936 in Liverpool.
Figure 10b. Rate of new STI diagnoses (excluding chlamydia diagnoses in people aged 15 to 24 years) per 100,000 population aged 15 to 64 years among North West residents by upper tier local authority of residence, 2021
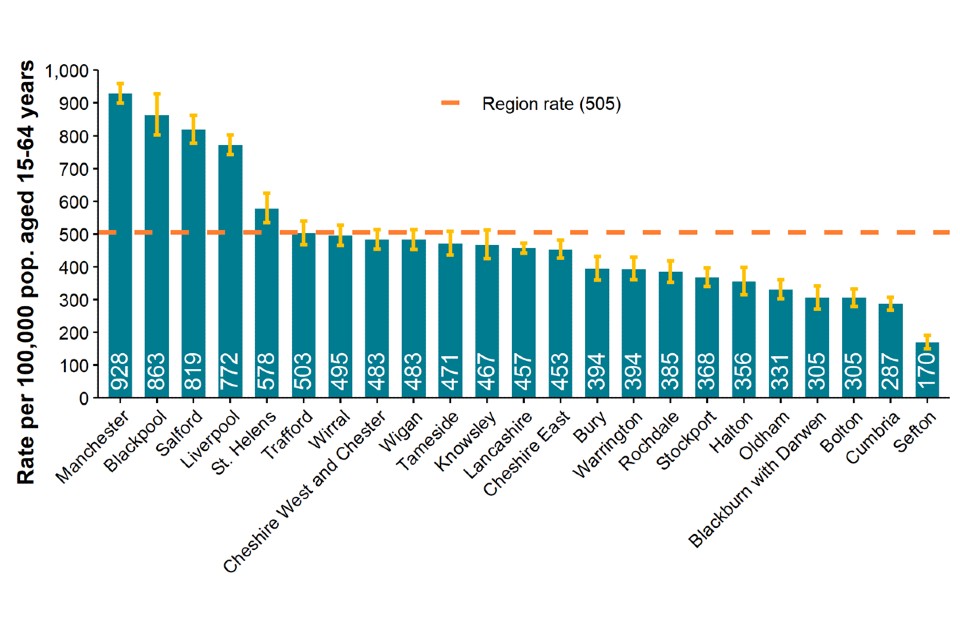
Data sources: GUMCAD, CTAD
Figure 10b is a bar chart showing the rate of new STI diagnoses (excluding chlamydia diagnoses in people aged 15 to 24 years) per 100,000 population aged 15 to 64 years among North West residents by local authority of residence in 2021. It shows the rate of new STIs (excluding chlamydia in young people aged 15 to 24 years) by North West local authority compared to the rate in the North West (505 per 100,000) in people aged 15 to 64 years. The rates in local authorities ranged from 170 per 100,000 in Sefton to 928 per 100,000 in Manchester.
Figure 11. Chlamydia detection rate per 100,000 population aged 15 to 24 years in North West residents by upper tier local authority of residence, 2021
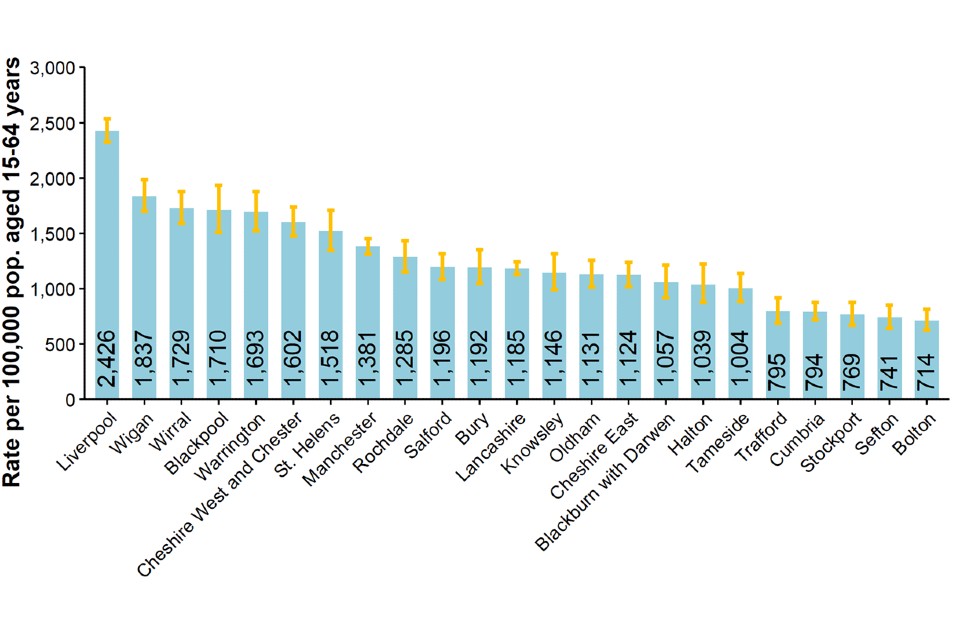
Data sources: GUMCAD, CTAD
Figure 11 is a bar chart showing the chlamydia detection rate per 100,000 population aged 15 to 24 years in North West residents by local authority of residence in 2021. It shows a large variation in the chlamydia detection rate in young people in North West local authorities from 714 per 100,000 in Bolton to 2,426 in Liverpool.
Figure 12. Rate of gonorrhoea diagnoses per 100,000 population in North West residents by upper tier local authority of residence, 2021
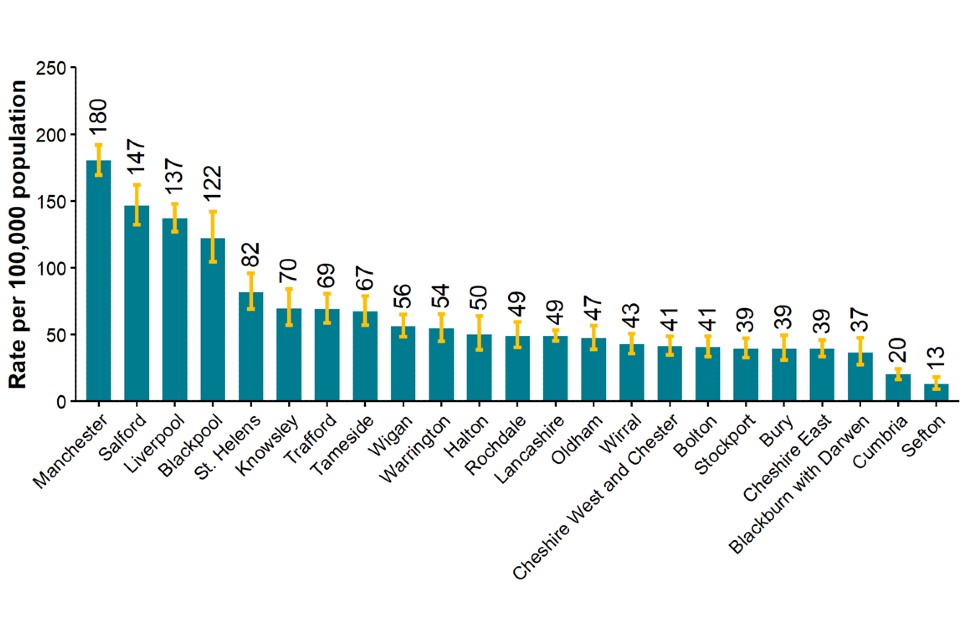
Data source: GUMCAD
Figure 12 is a bar chart showing the rate of gonorrhoea diagnoses per 100,000 population in North West residents by local authority of residence in 2021. It shows a large variation in the rate of gonorrhoea in North West local authorities from 13 per 100,000 in Sefton to 180 in Manchester.
Figure 13. Map of new STI rates per 100,000 residents by upper tier local authority in the North West, 2021
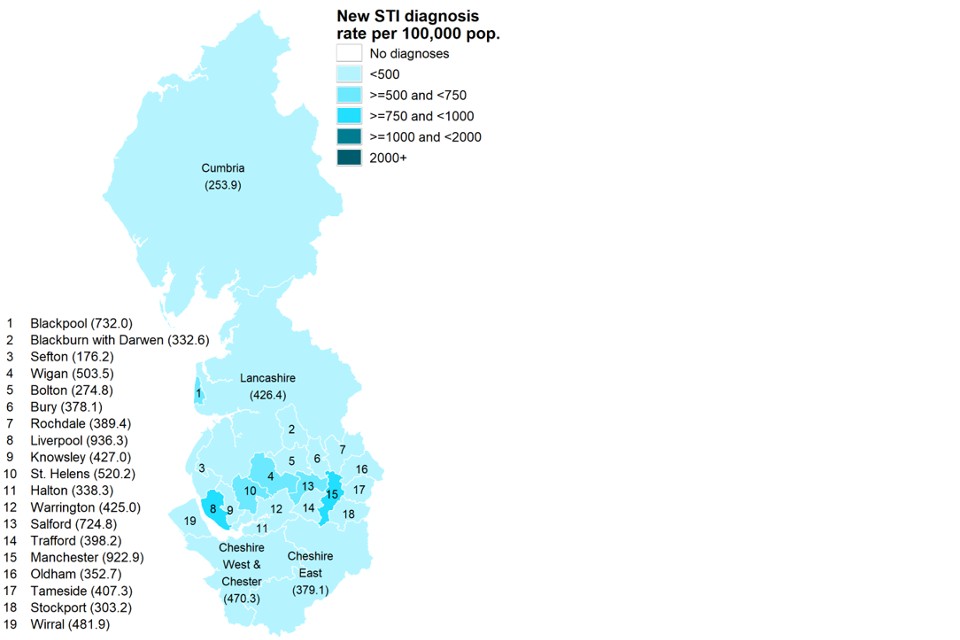
Data sources: GUMCAD, CTAD. Map contains Ordnance Survey data (© Crown copyright and database right 2021) and National Statistics data (© Crown copyright and database right 2021)
Figure 13 is a map of new STI rates per 100,000 residents by local authority in the North West in 2021. In general, more urban areas of the North West had higher STI rates compared to more rural areas.
Figure 14. STI testing rate (excluding chlamydia in under 25 year olds) per 100,000 population in North West residents aged 15 to 64 years, 2017 to 2021

Data sources: GUMCAD, CTAD
Figure 14 shows trend lines for the STI testing rate (excluding chlamydia in under 25 year olds) per 100,000 population in the North West and England residents aged 15 to 64 years from 2017 to 2021. After a rise in testing from 2017 to 2019 in both the North West and England, the testing rate fell from 2019 to 2020, and increased again from 2020 to 2021. The testing rate in the North West remained lower than the rate in England throughout.
Figure 15. STI testing positivity rate [note 5] (excluding chlamydia in under 25 year olds) in North West residents, 2017 to 2021
Data sources: GUMCAD, CTAD
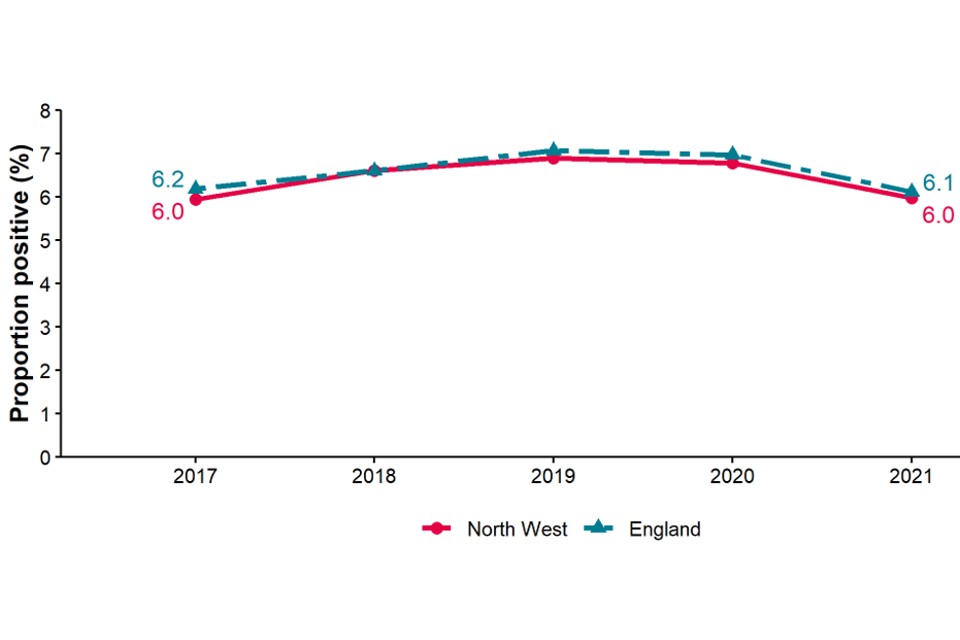
Data sources: GUMCAD, CTAD
[note 5] The numerator for the STI testing positivity rate now only includes infections which are also included in the denominator. These are: chlamydia (excluding diagnoses in those aged under 25 years), gonorrhoea, syphilis and HIV. Up to 2018 (data for 2017) it included all new STIs.
Figure 15 shows trend lines for the STI positivity rate (excluding chlamydia in those aged under 25 years) in the North West and England residents from 2017 to 2021. It shows that North West positivity was slightly lower than England, and both remained roughly stable (between 6% and 7%) from 2017 to 2021.
Table 4. Number of diagnoses of new STIs by UKHSA region of residence, data source and data subset 2021
| UKHSA region of residence | GUMCAD specialist SHSs | GUMCAD non-specialist SHSs [note 6] | CTAD [note 7] | Total |
|---|---|---|---|---|
| East Midlands | 10,622 | 6,275 | 3,974 | 20,871 |
| East of England | 15,809 | 4,238 | 5,608 | 25,655 |
| London | 69,545 | 8,162 | 23,792 | 101,499 |
| North East | 7,495 | 1,580 | 2,718 | 11,793 |
| North West | 23,693 | 3,789 | 7,954 | 35,436 |
| South East | 26,578 | 1,960 | 8,287 | 36,825 |
| South West | 13,797 | 2,444 | 4,782 | 21,023 |
| West Midlands | 16,890 | 3,867 | 4,804 | 25,561 |
| Yorkshire and Humber | 16,031 | 2,050 | 7,724 | 25,805 |
Data sources: GUMCAD, CTAD
[note 6] Diagnoses from enhanced GPs reporting to GUMCAD are included in the ‘Non-specialist SHSs’ total.
[note 7] Including site type 12 chlamydia from GUMCAD.
Table 4 shows the number of diagnoses of new STIs by UKHSA region of residence, data source and data subset in 2021. It shows that the highest number of STIs were diagnosed in London residents, with the majority of new STIs being diagnosed in specialist SHSs.
Table 5. Number of diagnoses of the 5 main STIs in the North West by STI, data source and data subset 2021
| 5 main STIs | GUMCAD: specialist SHSs | GUMCAD: non-specialist SHSs [note 8] | CTAD [note 9] | Total |
|---|---|---|---|---|
| Syphilis | 798 | 11 | 809 | |
| Gonorrhoea | 4,294 | 642 | 4,936 | |
| Chlamydia | 8,738 | 2,857 | 7,954 | 19,549 |
| Genital herpes | 2,341 | 77 | 2,418 | |
| Genital warts | 3,108 | 66 | 3,174 |
Data sources: GUMCAD, CTAD
[note 8] Diagnoses from enhanced GPs reporting to GUMCAD are included in the ‘Non-specialist SHSs’ total.
[note 9] Including site type 12 chlamydia from GUMCAD.
Table 5 shows the number of diagnoses of the 5 main STIs in the North West by STI, data source and data subset in 2021. It shows that the majority of new STIs are diagnosed in specialist SHSs.
Information on data sources
Find more information on local sexual health data sources on GOV.UK.
These figures are based on data from the GUMCAD and CTAD surveillance systems published on 4 October 2022 (data to the end of calendar year 2021).
GUMCAD surveillance system
This disaggregate reporting system collects information about attendances and diagnoses at specialist (level 3) and non-specialist (level 2) SHSs. Information about the patient’s area of residence is collected along with demographic data and other variables. GUMCAD superseded the earlier KC60 system and can provide data from 2009 onwards. GUMCAD is the main source of data for this report.
Due to limits on how much personally identifiable information SHCs are able to share, it is not possible to deduplicate between different clinics. There is a possibility that some patients may be counted more than once if they are diagnosed with the same infection (for infection specific analyses) or a new STI of any type (for new STI analyses) at different clinics during the same calendar year.
CTAD surveillance system
CTAD collects data on all NHS and local authority or NHS-commissioned chlamydia testing carried out in England. CTAD is comprised of all chlamydia (NAATs) tests for all ages (with the exception of conjunctival samples), from all venues and for all reasons. CTAD enables unified, comprehensive reporting of all chlamydia data, to effectively monitor the impact of the NCSP through estimation of the coverage of population screening, proportion of all tests that are positive and detection rates.
For services which report to GUMCAD and for which CTAD does not receive data on the patient’s area of residence (for example, SHSs), information about chlamydia diagnoses is sourced from GUMCAD data.
New STIs
New STI diagnoses comprise diagnoses of the following:
- chancroid
- Lymphogranuloma venereum (LGV)
- donovanosis
- chlamydia
- gonorrhoea
- genital herpes (first episode)
- HIV (acute and AIDS defining)
- Molluscum contagiosum
- non-specific genital infection (NSGI)
- non-specific pelvic inflammatory disease (PID) and epididymitis
- chlamydial PID and epididymitis (presented in chlamydia total)
- gonococcal PID and epididymitis (presented in gonorrhoea total)
- scabies
- pediculosis pubis
- syphilis (primary, secondary and early latent)
- trichomoniasis and genital warts (first episode)
- Mycoplasma genitalium
- shigella
Calculations
Confidence Intervals were calculated using Byar’s method.
Office for National Statistic (ONS) mid-year population estimates for 2020 were used as a denominator for rates for 2021. ONS ceased producing estimates of population by ethnicity in 2011. Estimates for that year were used as a denominator for rates for 2021.
Further information
As of 2020, all analyses for this report include data from non-specialist (level 2) SHSs and enhanced GP services as well as specialist (level 3) SHSs.
For further information, access the online Sexual and Reproductive Health Profiles.
Find more information on local sexual health data sources on GOV.UK.
Local authorities have access to the Summary Profile of Local Authority Sexual Health (SPLASH) Reports (accessible from the Sexual and Reproductive Health Profiles) and the SPLASH supplement reports via the HIV and STI Data exchange.
For an Annual Epidemiological Spotlight on HIV in the North West, contact [email protected]
About the Field Service
The Field Service was established in 2018 as a national service comprising geographically dispersed multi-disciplinary teams integrating expertise in Field Epidemiology, Real-time Syndromic Surveillance, Public Health Microbiology and Food, Water and Environmental Microbiology to strengthen the surveillance, intelligence and response functions of UKHSA. The Field Service also leads and coordinates the Global Health work of UKHSA’s National Infection Service working with the Global Public Health Team and will lead and coordinate the national aspects of UKHSA’s port health functions.
You can contact your local Field Service team at [email protected]
If you have any comments or feedback regarding this report or the Field Service, contact [email protected]
Acknowledgements
We would like to thank:
- local SHSs for supplying the SHS data
- local laboratories for supplying the CTAD data
- the UKHSA Blood Safety, Hepatitis, STI and HIV Division for collection, analysis and distribution of data
References
1. Mitchell KR, Shimonovich M, Bosó Pérez R, Dema E, Clifton S, Riddell J and others. ‘Initial Impacts of COVID-19 on sex life and relationship quality in steady relationships in Britain: Findings from a large, quasi-representative Survey (Natsal-COVID)’ The Journal of Sex Research March 2022: pages 1 to 12 (accessed 11 August 2022)
2. Howarth A, Saunders J, Reid D, Kelly I, Wayal S, Weatherburn P, Hughes G, and Mercer C. ‘Stay at home … Exploring the impact of the COVID-19 public health response on sexual behaviour and health service use among men who have sex with men: findings from a large online survey in the United Kingdom’ Sexually Transmitted Infections July 2022: pages 346 to 352 (accessed 11 August 2022)
3. Dema E, Gibbs J, Clifton S and others. ‘Initial impacts of COVID-19 on sexual and reproductive health service use and unmet need in Britain: findings from a large, quasirepresentative survey (Natsal-COVID)’ The Lancet Public Health January 2022: volume 7, pages e36 to 47
4. Sonnenberg P, Menezes D, Freeman L and others. ‘Intimate physical contact between people from different households during the COVID-19 pandemic: a mixed-methods study from a large, quasi-representative survey (Natsal-Covid)’. British Medical Journal Open February 2022: volume 12, issue 2 (accessed 11 August 2022)
5. Ratna N, Dema E, Conolly A and others. ‘O16 Ethnic variations in sexual risk behaviour, sexual health service use and unmet need during the first year of the COVID-19 pandemic: an analysis of population-based survey and surveillance data’. Sexually Transmitted Infections. 2022, volume 98: pages A8 to A9 (accessed 11 August 2022)
6. Sumray K, Lloyd KC, Estcourt CS, Burns F and Gibbs J. ‘Access to, usage and clinical outcomes of, online postal sexually transmitted infection services: a scoping review’ Sexually Transmitted Infections June 2022: pages 1 to 8 (accessed 11 August 2022)
