State of the environment: health, people and the environment
Updated 26 January 2023
Applies to England
Chair’s foreword
The coronavirus (COVID-19) pandemic has exposed and amplified green inequality in society. Too many towns and cities in England, especially those with a strong industrial heritage, have too little green space, too few trees, culverted rivers, poor air quality and are at risk of flooding. This holds back economic growth and the building of new homes. It’s also a fundamental moral issue. Areas of higher deprivation and Black, Asian and Minority Ethnic populations have less access to high quality green and blue space and this contributes to differing disease burdens and life expectancy.
Creating, and connecting people with, green or blue spaces will support new local jobs and benefit health and wellbeing. This is why it is important that the recovery from coronavirus is a green recovery. The pandemic has led to an increased appreciation of nature and more engagement with the water environment, we need to build on this revitalised interest in the natural world to achieve something that is better and that lasts.
In June, the Prime Minister said the way back from the economic impacts of the coronavirus pandemic was to “Build, Build, Build”. This caused some alarm amongst environmentalists, but building back “better, greener, and faster” is an opportunity to make development healthier. If the government wants to bring about a step-change in the nation’s health, planning reform could be a golden opportunity.
The Environment Agency works to speed up sustainable development by helping developers meet regulatory requirements efficiently, providing advice so they get it right first time. It is encouraging to see house builders revisiting plans in light of coronavirus with a focus on providing more and better quality green and blue spaces. The government is right to emphasise “levelling up”; access to such spaces for all adults and children is vital to that.
Air pollution today remains the single biggest environmental threat to health in the UK, shortening tens of thousands of lives each year. Even during the industrial revolution, the Victorians realised that parks would provide cities with “lungs”. Today our ambition can be greater than that: let’s Build, Build, Build in ways that will help people to Breathe, Breathe, Breathe.
Steered by the ambition of the 25 Year Environment Plan, the principle of net gain, and the idea of natural capital, we can improve the country’s health through the choices government, businesses and individuals make. These range from multibillion-pound investments in green infrastructure and procurement, to healthy choices such as walking and cycling to work, or putting in place property level resilience to reduce the disruption caused by flooding, which is known to have significant mental health impacts.
In June, Dr Maria Neira, Director of Environment, Climate Change and Health at the World Health Organization, said:
The world has gathered around one goal: the race to zero deaths from COVID-19. A healthy recovery from this pandemic means we need to continue and expand this race to zero deaths from climate change and environmental pollution, a race to zero people pushed into poverty because of health costs, to zero people breathing polluted air.
Through regulation of the waste, water, nuclear and carbon intensive industries, through our flood resilience work, and by heading to net zero by 2030, the Environment Agency is reducing emissions from industry, creating cleaner rivers and bathing waters, and helping to mitigate the worst impacts of climate change. There are some great examples in this report. Our work to connect people on the Fylde coast to their beaches has drawn on social prescribing through doctors’ surgeries; we have restored Middlesbrough’s becks to connect the community with water and wildlife, and we are helping people find rest and relaxation outdoors through angling.
The physical and mental health of everyone depends on quality green and blue space, and it reduces the burden on the NHS. At a time when there is such widespread recognition of these essential facts, we should value work to protect and enhance the natural world highly.
Thank you to the team for this timely report.

Emma Howard Boyd, Chair of the Environment Agency
Main findings
- Air pollution is the single biggest environmental threat to health in the UK, shortening tens of thousands of lives each year.
- After air pollution, noise causes the second highest pollution-related burden of disease in Europe, and is responsible for more life years lost than lead, ozone or dioxins.
- There is emerging evidence of health effects from lower levels of pollution, although these are not currently well understood.
- Antimicrobial resistant microbes are becoming more common in the environment due to contamination, meaning infectious illnesses may become harder to treat.
- Mental health conditions are increasing - they are the largest single cause of disability in the UK, and can be caused or affected by pollution, flooding and climate change.
- There is substantial and growing evidence for the physical and mental health benefits of spending time in the natural environment, but children are engaging less with nature.
- Exposure to pollution, and access to the natural environment are not equally distributed across society - people living in deprived areas often have poorer quality environments with less accessible green space.
- Equality of access to, and connection with, a healthy natural environment would save billions of pounds in healthcare costs and reduced economic activity every year.
- There are opportunities to improve health through the choices government, regulators, businesses and individuals make in creating and contributing to healthier, greener and more accessible environments.
Introduction
Note that preparation of this report started before the COVID-19 pandemic. References to COVID-19 are still the subject of much research and investigation.
This report focuses on the relationship between human health and people’s access to and connection with a clean, high quality natural environment. It presents information on England’s environment, and people’s exposure to environmental pollutants, flooding and climate change in relation to human health. It highlights environmental inequalities that contribute to differences in health outcomes for people in England. Case studies throughout the report demonstrate the role played by the Environment Agency in protecting and enhancing the environment, and how this benefits people’s health.
Health is often understood in different ways by different people. In 1948 the World Health Organization (WHO) defined health as ‘a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity’[footnote 1]. Wellbeing includes people’s satisfaction with life, and their feelings that the things they do in their life are worthwhile[footnote 2]. This view allows people to experience good health at all life stages and even during some physical illness[footnote 3]. Human health is affected by the surrounding environment in many and complex ways (figure 1).
Pollution can damage people’s health throughout their lives and even before birth. Scientific research is revealing more about the connections between human health and the quality of the environment. It is beginning to identify the mechanisms by which people’s exposure to and interaction with the natural environment can affect their wellbeing. There is increasing recognition that human health depends ultimately on the health of the natural world, its species and ecosystems.
Figure 1: determinants of human health and wellbeing
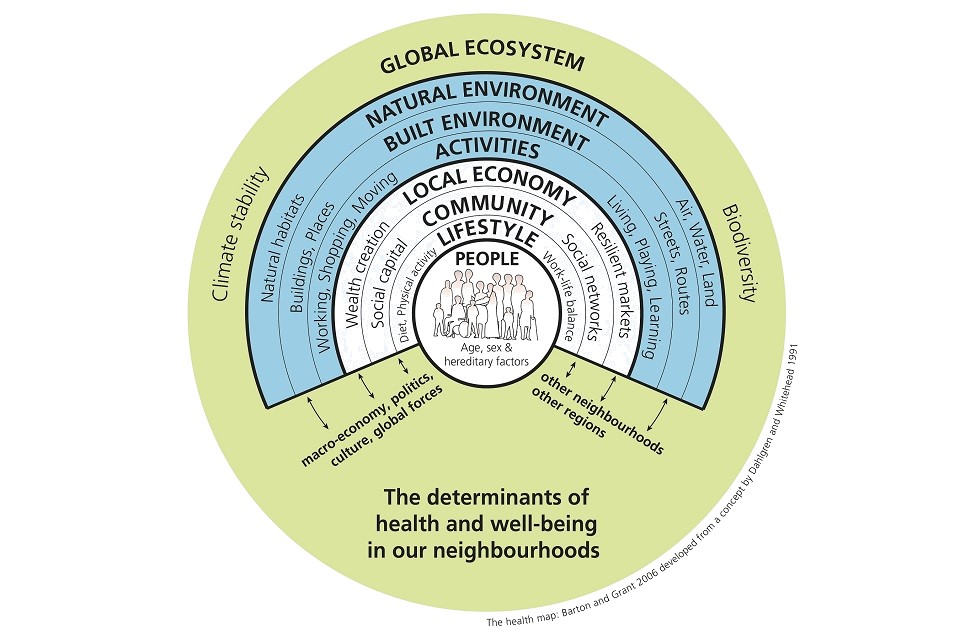
Copyright © 2006 by SAGE Publications, Ltd. Reprinted by Permission of SAGE Publications, Ltd.
Environmental pollution and health
The health benefits of clean air, land and water have been recognised by people throughout history and across cultures. England’s rapid industrialisation and urbanisation led city-dwelling Victorians to flock to the coast and countryside to improve their health and wellbeing and escape polluted cities. Also during this time, the introduction of sewers and indoor plumbing revolutionised public health, forming the basis of modern sanitation and drinking water systems.
Since the 1950s, legislation and regulation have reduced industrial emissions and made England’s air, land and waters safer and cleaner. Some pollutants, however, are posing increasing risks, or finding new routes into the environment. For example, changes to the composition and treatment of waste, have led to new challenges in preventing soil contamination from spreading of treated sewage and other biowaste.
Many pollutants can affect health through long-term, low level exposure. Knowledge of these processes is still in its early stages. Further research into the potential health effects of long-term, low level exposure to synthetic chemicals is required. Antimicrobial resistant bacteria are becoming widespread in the environment and pose a serious and rapidly growing threat to human health. Emerging pollutants such as microplastics and nanomaterials potentially pose new risks to health which we need to understand.
Despite the many gaps in the understanding of the effects of environmental pollution on health, it is known that the contribution to the overall burden of disease is significant. The World Health Organization estimate that environmental factors contribute about 14% of the total burden of disease in the United Kingdom[footnote 4].
Air pollution
Air pollution is the single greatest environmental threat to health in the UK[footnote 5]. Air pollution can have short-term, immediate effects on health, such as wheezing and coughing, and can exacerbate pre-existing conditions. Long-term exposure to air pollutants in the UK shortens tens of thousands of lives every year and reduces average life expectancy by several months[footnote 6]. An estimated 5% of total mortality in England can be attributed to small particulate matter (PM2.5) alone[footnote 7]. Children, the elderly and those with pre-existing conditions are the most vulnerable to the health effects of air pollution[footnote 8].
Long-term exposure to air pollution has been associated with dementia, heart disease, stroke and some cancers[footnote 6]. Small particulate matter is inhaled and some of the smallest particles can enter the bloodstream, making it particularly harmful. The particles are transported in the blood, potentially exposing all cells in the body. Children’s development before and after birth can be affected. There is some emerging evidence that these effects could include the development of the brain[footnote 9]. Air pollution may also affect both susceptibility to infections and the effectiveness of the antibiotics used to treat them[footnote 10]. Air pollution can cause chronic diseases. Some of these have been identified as increasing the risk of severe COVID-19 symptoms. It has been suggested that there may be an association between levels of air pollution and the severity of COVID-19 symptoms. Further work is required to clarify the magnitude of this association[footnote 11].
Emissions of some air pollutants have massively reduced over recent decades as a result of improved technology, environmental policy and regulation[footnote 12]. This has had significant health benefits. Figure 2 shows that the number of UK deaths attributable to long-term nitrogen dioxide (NO2) and PM2.5 exposure reduced by 44% and 56% respectively between 1970 and 2010[footnote 13].
Figure 2: fraction of all deaths attributable to long-term exposure to NO2 and PM2.5
| Year | % mortality rate NO2 | % mortality rate PM2.5 |
|---|---|---|
| 1970 | 5.32 | 11.83 |
| 1980 | 5.44 | 10.50 |
| 1990 | 5.76 | 9.50 |
| 2000 | 4.19 | 6.90 |
| 2010 | 2.96 | 5.21 |
Source: Carnell, E. and others, 2019
Road transport and household wood burning are major contributors to outdoor air pollution and pollution remains at illegal levels in some roadside locations[footnote 14].
Particulate matter and NO2 alone have been estimated to have health costs of around £22.6 billion every year[footnote 9]. Poor health associated with, or exacerbated by, air pollution leads to time off work and reduced productivity. Illness associated with air pollution affects children’s education and can lead to fewer employment options in adult life.
Ammonia emissions, mainly from agriculture, can cause localised odour issues in rural areas[footnote 15]. Ammonia combines with other pollutants in the atmosphere to form secondary particulate matter. This particulate matter can be transported across large distances, with associated health effects on a wide population[footnote 12]. Ammonia emissions have been increasing in the UK since 2013, although this reverses the trend of a long-term decrease since 1998[footnote 16].
Ozone is a secondary pollutant formed when other air pollutants react with each other in the atmosphere. It is a significant hazard to health in the UK in some areas during the summer months[footnote 17]. It causes respiratory problems and increased numbers of hospital admissions when levels are high. Background levels of ozone have increased in rural and urban areas over recent decades[footnote 18].
Indoor air pollution, caused by open fires, wood burning stoves, cooking and use of household products containing chemicals, is also a major contributor to ill health[footnote 18].
Water pollution
Everyone in England has access to safely managed drinking water supplies. The introduction of sanitation measures, such as piped water and sewage management, in the 19th century prevented deaths from water-borne diseases. It’s difficult to know how many lives have been saved in England through sanitation, but it’s estimated that worldwide, lack of safe drinking water and sanitation is responsible for around 1.6 million deaths every year[footnote 19].
Groundwaters, which supply around 30% of the country’s drinking water[footnote 20] have been deteriorating in quality over the last 60 years[footnote 21]. A major cause of this is nitrates from agriculture. Nitrate limits for drinking water are set to prevent methaemoglobinaemia (‘blue baby’ syndrome) and thyroid impacts in bottle fed babies, who are the most vulnerable population. These limits are based on short-term effects but are also considered protective for any long-term effects[footnote 22]. Nitrate levels in UK drinking water do not exceed international thresholds for health protection although sometimes this is managed by blending of water sources.
The quality of England’s surface water bodies has generally improved over recent decades, but progress has not continued in recent years[footnote 21]. Coastal and inland waters can become contaminated by microorganisms from sewage, livestock and wildlife, which can cause infections. The quality of designated coastal bathing waters in England is assessed by measuring the levels of certain bacteria. Figure 3 shows that bathing water quality has improved over the last 30 years, with 98.3% passing minimum standards and 71.4% at excellent status in 2019.
Figure 3: trend in bathing water classification 1995 to 2019
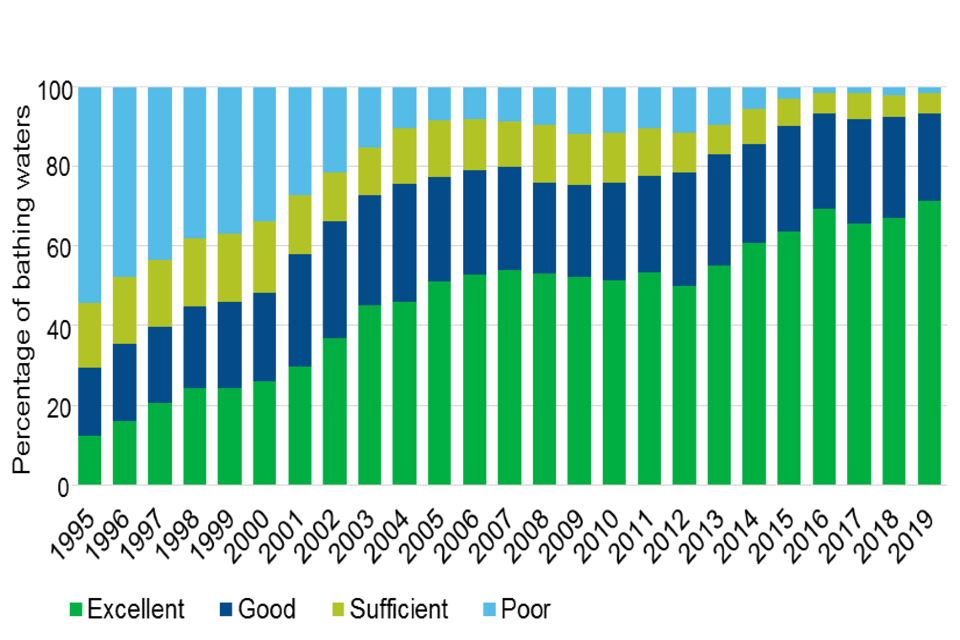
Bathing and use of designated bathing beaches is only one of the water-contact activities in the UK. Other water sports, including wild swimming in rivers and lakes, are increasing in popularity and often in areas not covered by protective water quality legislation.
Chemicals
Chemicals are used by everyone, every day. Many of these products are beneficial to society and have brought improvements in health, hygiene and safety. The health risks of many substances are assessed by chemical companies or regulatory bodies in accordance with legislation, and are reviewed if new knowledge emerges. In some cases, the decision to allow chemicals to be used depends on whether safer alternative products are available.
Chemicals enter the wider environment through pathways including:
- industrial and transport emissions to air, and their deposition to land and water
- urban drainage and waste water
- run-off of pesticides from the land to water bodies
- spreading of manures and sewage sludge to soils
- run-off of metallic mining waste to water bodies
Synthetic chemicals
Synthetic chemicals are used very widely, including in agriculture, healthcare and in people’s homes and workplaces. Products containing synthetic chemicals include paints, plastics, cleaning and personal care products and fire retardant furniture.
Since 1950, more than 140,000 new chemicals have been synthesised globally. Those produced in the largest amounts are now dispersed throughout the environment, and people worldwide are exposed to them[footnote 23]. A large number of new chemicals are produced and used each year, and it takes time to build up evidence on their hazards and risks. In addition, most chemicals degrade over time, and information on the by-products of this degradation are not always available. To date over 22,000 different synthetic chemicals have been registered in Europe as being produced in volumes over one tonne a year[footnote 24]. In 2017, 81 million tonnes of chemicals hazardous to the environment were produced in Europe, including the UK[footnote 25].
Relatively little is known about the long-term health effects of many common pollutants that people are exposed to at low levels in the home and the wider environment. There is no strong evidence that everyday, low-level exposure to synthetic chemicals is causing health effects, but more research is needed. Acute toxic effects are easier to study and are therefore better understood than the effects of long term, low-level exposure.
Some of the chemical groups of greatest health concern are:
- bisphenol A and phthalates, used in plastics manufacturing[footnote 8]
- perfluorinated compounds (PFCs), used in a wide range of products such as stain- and water-repellent fabric coatings, and non-stick cooking equipment[footnote 26]
- dioxins and polychlorinated biphenyls (PCBs), which are by-products from a range of industrial sectors[footnote 27] and are also released through uncontrolled burning such as household coal and wood fires[footnote 28]
These chemical groups are of great concern because of their potential effects, such as interference with hormones. Many chemicals are designed not to breakdown and can therefore persist in the environment for a long time. Many of them also accumulate in the tissues of humans and animals, becoming more concentrated as they travel up through the food chain[footnote 3]. People are continually exposed to them at low levels in the environment and via food. Human milk is a good way to monitor background levels in the population. European data shows that levels of dioxins in human milk have been declining over recent decades as a result of better industrial regulation and cleaner technologies[footnote 29].
There is also growing evidence that the mixtures of chemicals people are exposed to can pose risks to health that cannot be predicted from their individual properties. Some people will be more susceptible to the effects of chemicals as a result of natural genetic variation among individuals[footnote 8].
Growth and innovation in the chemical industry will increase levels of synthetic chemicals in the environment. Global chemical production has almost doubled since 2000 and is anticipated to continue growing[footnote 30]. This will create research and regulatory challenges in ensuring the risks to human health are minimised.
Case study - Regulating the chemical industry
The Environment Agency works with the Health and Safety Executive to assess the risks of chemicals under the REACH Regulation. By law, chemical companies are responsible for demonstrating that their chemicals can be used safely. We work with other organisations, providing advice on when to instruct companies to perform additional testing and impose additional controls where we think they have not gone far enough.
We develop environmental quality standards for the water environment to protect people and wildlife from the harmful effects of chemicals. We have also produced guidance to allow local authorities and others to assess the health impacts of contaminated land.
More broadly, we also regulate chemical emissions to air, land and water, using Emission Limit Values. These standards are developed at European, UK and local levels, working with Public Health England and others.
Metals
Metals are present everywhere in the environment, and come from both natural and manmade sources. Some metals in very low quantities, for example iron, are essential to help our bodies to function properly. Others can be very harmful and they are monitored and controlled in order to protect public health. Some metals accumulate in the body over time and can cause adverse health effects on the nervous, respiratory, immune and other body systems. Industrial and municipal emissions of historically used toxic metals such as lead and mercury are in decline as a result of regulation[footnote 14]. Even when emissions have stopped completely, levels can remain elevated for long periods. This is often found in urban soils, and land and water affected by historical mining.
Advances in technologies have also seen emerging elements such as the rare earths and lithium being increasingly used. Understanding of how they behave in the environment, and their effects on health is still in its early stages.
Exposure to some metals is increasing as a result of increasing amounts of road traffic. Brake wear produces particles of metals such as arsenic, nickel and copper, which can all be toxic at certain doses. The particles are so small that they are capable of entering the lungs with some being absorbed into the bloodstream[footnote 8].
Emerging pollutants
A pollutant is considered to be ‘emerging’ if it is either a new presence in the environment or it is newly understood to be a hazard to the environment or human health. For example, understanding of the human health impacts of microplastics, which enter people’s bodies via the air, land and water environments, is still at a very early stage[footnote 31]. Some of the main sources of microplastics in the environment are:
- synthetic fabrics
- road marking paints
- packaging products
- road vehicle tyres
Nanoparticles are increasingly common in everyday items such as sunscreens and cosmetics, as well as in anti-fouling boat paints. They can enter the water environment and can have negative effects on aquatic life[footnote 21]. The effects on human health are less well understood.
Antimicrobial resistance (AMR) in the environment
The modern world depends heavily on effective healthcare to limit illness and premature deaths in humans, and effective control of livestock diseases. Central to both of these is the use of antimicrobial substances such as antibiotics and antifungals to treat infectious diseases and to protect people following procedures such as surgery and chemotherapy. Through genetic changes, antimicrobial resistance can occur naturally over time. The overuse of antimicrobials in humans and livestock has accelerated this process leading to antimicrobials resistant microbes arising, persisting and spreading in the environment[footnote 32]. These microbes include:
- bacteria, linked to rising resistance to tuberculosis drugs
- viruses, linked to rising resistance to HIV antiretrovirals and influenza antivirals
- protozoans, linked to rising resistance to antimalarial drugs
- fungi, linked to rising resistance to antifungal drugs
Resistant microbes are spread into the environment chiefly from sewage and agricultural waste[footnote 33]. Antimicrobial drugs are also released from these sources and can directly influence the evolution and selection of resistant organisms in the natural environment[footnote 34]. Manufacturing waste from the pharmaceutical industry can also be a source of these contaminants, although the scale of this is uncertain[footnote 32].
Antimicrobial drug resistant infections are becoming more common. In the past AMR was seen as a problem just for hospitals, but increasingly patients are acquiring resistant infections elsewhere[footnote 35]. Evidence suggests that the environment is a significant source and reservoir of AMR[footnote 33]. One UK study has linked exposure to AMR organisms in coastal waters to their colonisation of the guts of surfers. The study found antibiotic resistant E. coli in water samples from 11 out of 97 sampled bathing water locations. The resistant bacteria were also found to be carried by 6.3% of surfers sampled across all of the locations[footnote 35]. Little is known about how exposure to or colonisation by AMR microbes in the environment relate to immediate or future levels of resistant infections in humans.
Some countries are already approaching a situation where therapies that we take for granted simply no longer work[footnote 36]. In Europe, antibiotic-resistant infections kill at least 25,000 people every year[footnote 37]. A report commissioned by the UK government in 2014 estimated that this could rise to 390,000 by 2050. By then, antimicrobial resistant infections may be the leading cause of death worldwide[footnote 38].
The UK government has developed a national action plan to target antimicrobial use, develop new drugs and technologies, and control the spread of antimicrobial resistant organisms into the environment[footnote 39]. Without such large-scale, co-ordinated measures, AMR will cause people to suffer prolonged illness as common infections become more difficult to treat.
Odour
Odour is a significant environmental cause of public complaints, and has a negative effect on quality of life in affected communities[footnote 40]. People in affected communities often report higher levels of other health issues, particularly anxiety and stress-related illness[footnote 41]. Concentrations of odour-causing chemicals occasionally exceed odour thresholds at the boundaries of landfill sites, potentially leading to stress and anxiety amongst local populations.
The main sources of odour pollution across Europe are:
- agriculture
- industrial activity
- waste management (including illegal waste activity)
Noise
Noise causes the second highest pollution-related burden of disease in Western Europe after air pollution[footnote 8]. It is responsible for more life years lost than other pollutants such as lead, ozone and dioxins[footnote 42]. The main source of noise pollution is road traffic[footnote 3]. The 2012 National Noise Attitude Survey found that 8% of the population are very or extremely bothered, annoyed or disturbed by noise from road traffic[footnote 43]. Recent noise mapping data shows that the number of people in England exposed to road and railway traffic noise exceeding WHO guidelines is 11.5 million and 1.5 million, respectively[footnote 44].
Noise pollution has been linked to[footnote 45]:
- sleep disturbance
- severe chronic annoyance
- coronary heart disease
- metabolic health outcomes, such as diabetes and obesity
- disruption to children’s learning and development
One study has estimated the medical cost of noise-related hypertension and associated conditions in the UK at £1.09 billion a year[footnote 46]. The findings suggested that exposure to noise above recommended levels resulted in an extra 1,169 cases of dementia, 788 strokes and 542 heart attacks over the year studied. The total social cost of road traffic noise pollution, including health costs, productivity losses and chronic severe annoyance, has been estimated to be more than £9 billion annually[footnote 47].
Light pollution
Obtrusive artificial light causes stress, sleep interruptions and disrupts people’s enjoyment of the night sky and the countryside. It can usually be prevented by the correct design and positioning of lights[footnote 48].
Bioaerosols
Bioaerosols are airborne particulates of biological origin, such as bacteria and fungal spores. They occur naturally in the environment as well as being emitted by certain human activities. Different combinations of particles are found in different places.
Emissions of bioaerosols, mainly from intensive livestock, composting facilities and spreading of manure and slurry, are sometimes a concern for people living in the surrounding area. Some studies suggest that people living near composting facilities, and children near intensive farming sites may be at increased risk of immune reactions such as asthma[footnote 49]. However, there is also a small amount of evidence that some bioaerosol mixtures may have beneficial effects on children’s developing immune systems[footnote 8].
Case study - Taking action on bioaerosols
Public concern around potential health impacts of bioaerosols from waste sites and farms has led the Environment Agency to gather evidence on the type and scale of any such impacts. While the research is being carried out we have taken a precautionary approach to regulating the industries involved. We minimise any risk to those living nearby by setting stringent limits on emissions. We are working with Public Health England to better understand potential health risks so that we can move from a precautionary to a risk-based regulatory approach. This will ensure that we can regulate businesses fairly and proportionately while protecting the public.
Radiation
Ionising radiation
Ionising radiation consists of particles, X-rays or gamma rays with enough energy to cause ionisation in the medium through which they travel. The ionised particles can cause damage to surrounding tissues, including DNA damage. The radiation can arise from radioactive materials or cosmic radiation. People are exposed to ionising radiation from a range of natural and human-made sources (figure 4) [footnote 50].
Figure 4: UK population exposure from naturally occurring and artificial sources of ionising radiation
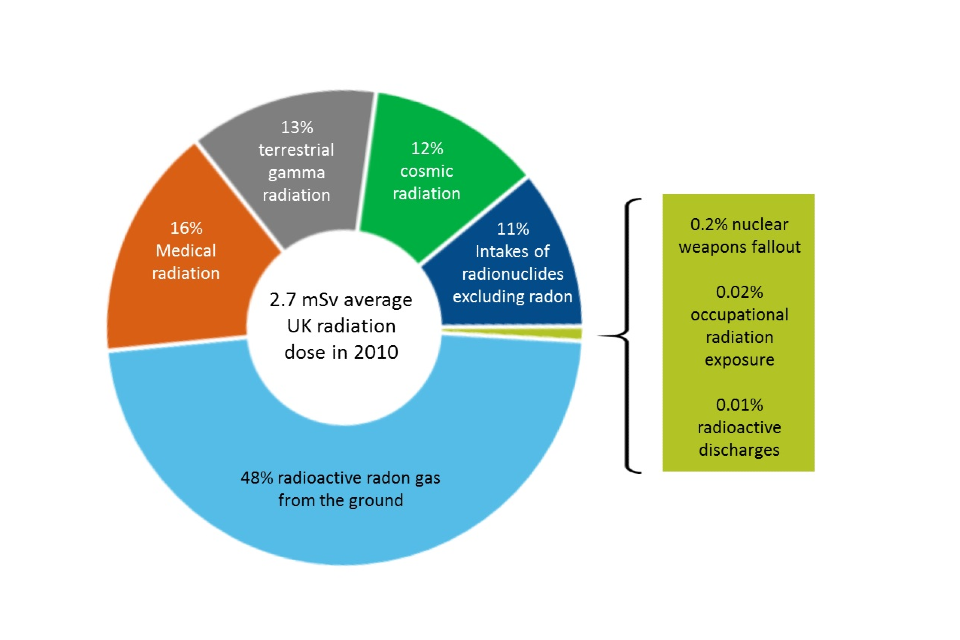
Source: Public Health England, licensed under Open Government Licence v3.0.
Natural and human-made ionising radiation both have the potential to cause cancer. The extra cancer risk to the UK public from the very low doses from human-made sources will be extremely small, and hard to detect within the population[footnote 51].
The average annual radiation dose to someone in the UK is 2.7 millisieverts (mSv), of which less than 0.01% is from radioactive discharges from industry. Actual doses vary across the country, depending mainly on the underlying geology that affects levels of naturally occurring radon gas in the air. Radiation doses to people living around nuclear licensed sites from authorised releases of radioactivity were well below the UK limit of one mSv a year when assessed in 2018[footnote 52].
Release limits are strict and are set to protect both people and the environment. Worry about exposure to radiation can have health consequences that are out of proportion to the actual risk to the public. Clear and accurate communication of this risk is very important to minimise unnecessary concern.
Non-ionising radiation
Non-ionising radiation includes:
- visible light
- ultra-violet light
- infra-red radiation
- electromagnetic fields
Sources of electromagnetic fields are used extensively in telecommunications and manufacturing. A large number of studies have been carried out over recent years, with no convincing evidence to suggest health impacts within international exposure guidelines[footnote 53]. Ultra-violet light is part of natural sunlight and also forms part of some man-made light sources. It can cause a number of health problems, including skin cancer.
Health benefits of the natural environment
Many people feel that spending time outdoors does them good mentally and physically. There is now a growing body of evidence which explains how people can benefit from contact with the natural world, which includes vegetated areas in and around cities as well as rivers, beaches and lakes. There has been a rise in the prominence of social prescribing, where clinicians have recognised the therapeutic benefits of spending time outdoors. They have prescribed walking, gardening or other activities to alleviate mental and physical ailments.
Recent evidence suggests that living in or near to greener environments reduces mortality rates and improves mental wellbeing[footnote 54]. A study of over 19,000 people in England looked at the effects of spending 2 hours or more a week in or around open green spaces. The results showed a significant increase in the likelihood of people reporting good health or high wellbeing[footnote 55].
Living near or visiting the coast or rivers and lakes increases people’s self-reported levels of mental health and wellbeing[footnote 56]. There is also evidence that living closer to these environments is associated with increased levels of physical activity. Proximity to the coast in particular has been found to increase overall health, and is associated with lower levels of being overweight[footnote 56]. These effects are present across different types of living environment (urban, urban fringe or rural) [footnote 57].
One study estimated that people with good access to the natural environment are 22% more likely to be physically active[footnote 58]. There is some uncertainty around this figure as physical activity is influenced by a range of factors.
People of all ages benefit from physical activity. It reduces the risk of mental illness, dementia, and physical conditions such as obesity, type 2 diabetes and heart disease[footnote 59]. In England obesity alone is responsible for more than 30,000 deaths and is estimated to cost society £27 billion every year[footnote 60]. The social benefits of physical activity in England have been valued at an estimated £2.18 billion a year, but this could be higher if more people had access to good places to exercise in[footnote 61].
Some studies have found that access to the natural environment increases social contact and community cohesion[footnote 62], which could be having a significant positive impact on health and wellbeing. The sensory experience of being immersed in the natural environment may play a part in the restorative effects on wellbeing. A study of beach visitors found that many people felt the sound of the waves along with other sensory inputs allowed them to clear the ‘noise’ from their minds. They reported that this created a sense of mental space and relaxation[footnote 63]. Three quarters of respondents to an RSPB public opinion survey said that nature has been important source of relief during the COVID-19 lockdown[footnote 64].
To some degree, the wellbeing benefits of spending time in the environment depend upon an individual’s sense of connection to nature. Regardless of overall time spent in the environment, people with a strong emotional and cognitive relationship with nature are more likely to state that their lives have meaning and purpose, than those without such a relationship[footnote 65].
Some of the positive effects of the natural environment may be increased when there are higher levels of species or ecosystem diversity[footnote 66]. There is evidence to suggest that exposure to biologically diverse ecosystems may influence the development of a healthy gut microbe community and the immune system in children[footnote 67]. Several studies have found that children living on farms, or in homes with more ‘farm-like’ bacteria in the house dust are less likely to develop asthma[footnote 68]. The bacteria are thought to derive from soil, livestock and household pets.
There is a growing focus on better understanding the natural environment and quantifying the true benefits to health. This can be done using a natural capital based approach. Natural capital accounting helps us measure those benefits people and wildlife receive from natural ‘assets’ such as woodland, parks and street trees. It helps us monitor change, inform decision making and protect them for future generations. The Greater Manchester “Urban Pioneer” project estimates that the city’s current natural capital will provide £9 billion in avoided health costs over the next 60 years.
Case study - North West Active Coast Programme
The Environment Agency carried out work to improve water quality along the north west coast in partnership with organisations including the National Farmers’ Union, water companies and local councils. The work also revealed that communities on the Fylde coast did not feel connected to their local beaches, seeing them as tourist destinations only.
The ‘LOVEmybeach’ Active Coast programme was launched in 2018, engaging local residents and schools, and linking to social prescribing through doctors’ surgeries. So many people were successfully connected to their beaches by the programme that it has now been used as a model for planned programmes elsewhere in England and across Europe.
Case study - Angling and health
The Environment Agency supports angling in England by maintaining and enhancing fisheries. Activities include improving fish habitats, re-stocking following fish kills and preventing the spread of damaging non-native species.
A total of 22.5 million days were spent freshwater angling in England in 2015, contributing £1.46 billion to the economy and supporting 27,000 jobs. Angling has been shown to have a multitude of health and social benefits, particularly for those with limited opportunities for other forms of physical exercise. Angling has double the number of participants with long-term illnesses compared to other sports. The vast majority of anglers cite rest and relaxation as an important reason for their participation in the sport.
Environmental inequalities and health
Good health and wellbeing are not equally enjoyed across society. The term ‘health inequalities’ is used to describe these avoidable and unfair differences in health between groups of people or communities. The difference in life expectancy between the most and least deprived areas of England has grown since 2010[footnote 69]. The difference in healthy expectancy was around 19 years in the period between 2016 and 2018[footnote 70].
Inequalities in environmental quality and accessibility all contribute to health inequalities in England. The poorest people often live and work in the most polluted environments[footnote 71]. They also have higher rates of underlying health conditions that may make them more vulnerable to the effects of pollution. The government’s Chief Medical Officer stated in 2018 that if “everyone had the type of environment currently only available to the most affluent sections of society, people would live longer, healthier, more productive lives with fewer years of ill health.” [footnote 3] The NHS could save over £2 billion in treatment costs if everyone in England had equal access to good quality green space[footnote 72].
Analysis has shown that areas of highest deprivation and those with high proportions of ethnic minorities are disproportionately affected by high levels of air pollution[footnote 73]. In 2016, nitrogen dioxide exceeded legal limits in the nearest play spaces for 14% of under 16 year olds in Greater London. Two-thirds of these children lived in deprived areas[footnote 74].
People in the most deprived areas of England tend to have significantly less accessible green space in their locality than those living in wealthier areas[footnote 75]. Large areas of green space in deprived urban neighbourhoods often remain unused due to their poor quality. Perception of safety is the most important barrier to using local green spaces, as well as facilities such as toilets and cafes[footnote 76].
One study found that city communities with 40% or more black, Asian or ethnic minority residents have access to 11 times fewer green spaces locally than those comprising mainly white residents[footnote 76].
Access to the natural environment is essential for the health and wellbeing of people who would not exercise elsewhere. For example there are over 700,000 regular walkers who are unlikely to replace their walks with exercise elsewhere, should the accessibility or quality of their local environment decline. It is estimated that the loss of this space alone could lead to mortality and morbidity valued at over £450 million a year[footnote 77].
National survey data shows that more people are visiting the natural environment than ever before, with this trend applying broadly to adults across different sectors of society. Increases have been smaller among people of black, Asian and minority ethnic backgrounds[footnote 77] (figure 5).
Figure 5: frequency of visits to the natural environment (percentage of adults visiting at least once a week) by age, ethnicity and Index of Multiple Deprivation
| Year | Aged 65 and over | Black, Asian and minority ethnic | 10% most deprived areas, Index of Multiple Deprivation |
|---|---|---|---|
| 2009-2010 | 44% | 35% | 38% |
| 2010-2011 | 45% | 36% | 42% |
| 2011-2012 | 46% | 41% | 48% |
| 2012-2013 | 47% | 39% | 44% |
| 2013-2014 | 50% | 41% | 50% |
| 2014-2015 | 51% | 45% | 48% |
| 2015-2016 | 53% | 42% | 46% |
| 2016-2017 | 56% | 50% | 53% |
| 2017-2018 | 57% | 46% | 51% |
| 2018-2019 | 62% | 42% | 53% |
Source: Natural England.
Children are spending less time in the natural environment than those in recent generations. Less than 10% now play in natural places such as woodlands, countryside and heaths, compared to 40% of adults when they were young[footnote 79]. Natural England estimates that around 15% of children did not visit the natural environment at all in the year 2018 to 2019. This has increased from 12% in 2013 to 2014[footnote 80].
Predicted future increases in many chronic conditions such as diabetes, dementia and in obesity rates reflect deteriorating public health. There is an opportunity to promote better access to the natural environment to prevent and better manage ill health. As long as there are wider societal inequalities then these chronic conditions will continue to be exacerbated[footnote 81]. Climate change is likely to make these health inequalities worse with deprived communities more at risk due to poorer housing conditions. These communities are often in areas more likely to suffer from flooding and urban heat island effects, where urban developed areas retain heat and experience higher temperatures than nearby rural areas[footnote 70].
Case study - Middlesbrough becks
Middlesbrough’s becks are a network of small streams running through the city, and located in one of the most deprived areas in the country. The beck corridors break up the built-up areas and provide valuable wildlife habitats. In some places, the becks suffered from issues such as fly-tipping and anti-social behaviour. As a result, 95% of local people saw them as dirty, littered and unsafe areas and did not use them for leisure. Many of the watercourses had been altered from their natural structures, and were difficult to access.
Over 10 years, the Environment Agency worked with the local community, councils and wildlife trusts to improve the becks area by restoring and creating wildlife habitats and providing opportunities for fishing, boating and other leisure activities. The projects brought people together, increased use of the becks and reduced anti-social behaviour. A residents’ survey during the early years of the project found that 48% felt that the becks had become safer and more accessible. A park in one of the restored areas has been described as ‘a new heart’ of the community.
Flooding and health
There are relatively few injuries or deaths related to flooding in England, but flooding can have serious health effects, particularly on mental health. Physical health impacts are less common, but they can include shock, respiratory infections, high blood pressure and stomach upsets[footnote 82]. Floods are a greater risk to health if the water contains sewage or other contaminants[footnote 83].
One study found that rates of probable depression, anxiety and post-traumatic stress disorder (PTSD) were increased in people who had experienced a flood. Even one year after the flood, the study showed that one fifth of people were probably suffering from depression, over a quarter from anxiety and over a third were affected by PTSD[footnote 84]. After 2 years there was still an increased level of anxiety and depression in these people compared to the general population[footnote 85].
During flooding in England between November 2019 and February 2020, 4,600 properties were flooded, while 130,000 were protected by Environment Agency’s flood defences. It has been estimated that the mental health costs amounted to £20 million, though the mental health costs avoided due to the Environment Agency’s work is estimated at £590 million. The mental health impact is worse if people are displaced from their homes but less if people receive a flood warning in good time[footnote 86]. Some groups of people are more at risk from the impacts of flooding, including disabled people, the elderly and women[footnote 87].
Case study: Warrington’s flood defence scheme
The River Mersey flood alleviation scheme in Warrington, completed in 2018, benefits over 2,000 homes and businesses. The Environment Agency worked with others including local authorities to build 5km of flood wall and 2.2 km of embankment. The work also involved creating reed bed habitats, planting trees, opening up and connecting riverside paths, and improving views across the river and town. We have calculated the added value to human health in terms of the natural capital created by the project. The benefits from air quality improvement, recreation and physical activity alone add up to over £70 million over the lifetime of the scheme.
Climate change and health
England’s climate is changing and will continue to change as a result of greenhouse gas emissions. The Met Office’s Central England Temperature series shows that the 21st century has so far been warmer than the previous 3 centuries[footnote 88]. The summer of 2018 was the joint hottest ever recorded in the UK since 1910[footnote 89]. Hot summers, heatwaves and floods are all expected to become more frequent in future years[footnote 90].
It has been estimated that climate change has increased the likelihood of record breaking warm years in central England by at least 13 times[footnote 91]. There is evidence that heatwaves have been becoming more frequent over the past 150 years[footnote 92]. In the future, heatwaves are expected to last longer. The latest projections estimate that by the 2080s, a 10-day heatwave with daytime maximum temperatures over 30ºC will occur on average every 3 years[footnote 93].
Average annual rainfall in England has not changed since records began in the 18th century[footnote 88]. However, over the past 50 years, more winter rainfall has fallen in heavy events[footnote 94]. The projections also suggest that summers will be 16% to 46% drier than they are now. The impact of climate change on the frequency and intensity of extended droughts (lasting a year or more) remains unclear.
Future health impacts of climate change
The health impacts of a changing climate will mainly be felt through changes in temperature, disease and pollution[footnote 95]. High temperatures can affect health and cause premature death. Older people and those with underlying illnesses are more at risk and the numbers will increase with an ageing population as temperatures increase[footnote 95]. Heat related deaths may increase from 2,000 to 7,000 per year by the mid-2050s. Milder winters will reduce cold-related deaths by an estimated 2%[footnote 96]. This is likely to marginally reduce the total numbers of temperature related deaths overall, because there are so many more cold-related than heat-related deaths in the UK[footnote 97]. Hot weather is also known to increase aggressive and violent behaviour[footnote 98].
There may be an increase in frequency of episodes of high air pollution caused by weather patterns such as heatwaves[footnote 99]. There is evidence that pollen releases may increase, affecting hay fever symptoms. Higher temperatures will increase the suitability of the UK’s climate for invasive species and increase the risk of them spreading diseases[footnote 100]. Native disease vectors such as ticks and mosquitos may also increase in numbers or geographical range as temperature and moisture levels change[footnote 101]. For example, hot, dry weather can lead to increased areas of stagnant water, which would be likely to increase the spread of mosquito-borne diseases, should they be introduced. Land-use change such as creating wetlands may also contribute to mosquito abundance.
UK climate projections indicate that conditions increasing wildfire risk will become more common[footnote 102]. A review of the health effects of wildfires concluded that there is strong evidence that wildfire smoke exposure is associated with respiratory health effects. Growing evidence also suggests an association with increased mortality[footnote 103].
Over the next 50 years an increased frequency of flooding combined with a projected doubling of development on the flood plain could increase numbers of people affected. Careful planning and optimum investment implementation will minimise any increases in environmental stresses on people or properties in future housing developments[footnote 104]. This includes limiting the number of homes vulnerable to flooding and extreme temperatures.
Some communities in England are located in coastal areas where current defences cannot be sustained in the long term[footnote 105]. People in these communities may experience increased stress as a result of current or future impacts on their homes, businesses and families. The impacts of sea level rise also greatly increase the risk of economic decline in affected communities[footnote 106], increasing the likelihood of health inequalities.
Climate change and mental health
The impacts of climate change on mental health conditions such as anxiety and depression are becoming increasingly recognised[footnote 98]. A review of the global literature[footnote 107] suggests that some of these impacts can include:
- acute impacts of extreme weather events
- disruption to the social, economic and environmental systems that support mental health, particularly in vulnerable communities
- chronic stress, anxiety and guilt about future local and global climate change impacts
Human activity and health
Human activities have the potential to create pollution or other hazards to health. An individual’s exposure to these hazards and their impact on them varies according to where they live, their jobs and how they spend their leisure time.
Everyone’s life inevitably entails some risks, and everyone makes decisions and choices based on their own view of those risks. To make informed judgements about risks and benefits, people need access to the right information at the right time, as well as the skills to interpret it. Where this information is not provided, people will make decisions according to their own perceptions of risks and benefits. For example, many people enjoy leisure time in freshwater and coastal waters without information on water quality.
For many people, choices about their exposure to environmental hazards are determined by their limited options and not by the availability of information. This is influenced by wider socio-economic, health and cultural factors. For example, people in areas of high air pollution may not be able to move home, despite knowing the health risks they are exposed to.
The effects of long term exposure to pollutants and how they affect different people will be better understood in the future as analytical techniques and concepts develop further. Technological advances in wearable health monitors as well as improved health data collection, storage and access will increase people’s understanding of their own health. This could have positive effects on health through better awareness of their health status and increased motivation to spend time outdoors in the natural environment. This may be limited to those individuals with the economic means to engage with these technologies.
Zoonotic diseases
Zoonotic diseases are infectious diseases which are transmitted from animals to humans through pathogens such as viruses and bacteria. Humans and animals share many microorganisms, the vast majority of which do not cause diseases[footnote 108].
Around 75% of new and emerging infections are thought to have an animal origin[footnote 109]. There are a range of transmission pathways for these diseases. People working with animals or with animal products are most at risk of contracting these diseases, but food supplies can be contaminated with infected products, potentially exposing a much larger population[footnote 110].
Globally, the human and economic cost of zoonotic diseases can be huge. COVID-19 is a zoonotic disease, which likely originated from bat populations. As of July 2020, there have been over 15 million cases of COVID-19 and over 600,000 deaths, including over 45,000 deaths in the UK[footnote 111].
The main drivers of the emergence of zoonotic diseases are the increasing demand for meat and other animal products, unsustainable agricultural practises, and globalised food chains. Our consumption of agricultural products linked to unsustainable land use change, such as extensive deforestation, increases the risk of new zoonotic diseases emerging[footnote 108].
Case study - Monitoring pathogens in waste water
The Environment Agency is working in partnership with Bangor University to monitor levels of SARS-Cov-2 viral material in waste water. Since viral RNA fragments are shed in faeces, it may enter watercourses through sewage discharges of septic tanks, small and large treatment works and combined sewer overflows. The viral material itself is not infectious, but the results of this work will help public health experts understand levels of infections in the general population.
This approach is being employed around the world to study the development of the COVID-19 pandemic, and has potential as an early warning system for outbreaks. The technique could in future be applied to the detection and monitoring of other pathogens, including AMR organisms and water-borne diseases including gastrointestinal infections. There is also potential to improve water quality monitoring of important sites such as coastal bathing waters, and to develop better understanding of AMR in the environment. This reinforces the integral role of environmental surveillance in public health protection.
Conclusion
This report illustrates some of the great improvements that have been made in the quality of England’s air, land and water, tackling the polluted legacy of the Industrial Revolution. Regulation was introduced, to protect communities and the environment without imposing an undue burden on industry. Some problems have proved harder to solve than others. Along the way, new risks have arisen with new technologies and innovations, and changes in the way people live and work. Research continues to increase understanding of the sources, pathways and health impacts of pollutants, while regulation reduces harm caused. Behaviours which cause a high amount of pollution will have to change, particularly where they disproportionately affect the most vulnerable people in society. This could include choosing to walk, cycle or use public transport instead of driving.
The benefits of a healthy natural environment for mental and physical health are also clear. There are opportunities for strategic design and planning of communities that will enable people to live healthy, fulfilling lives, while protecting the nation’s natural environment. The economic benefits of doing so, in terms of health and social costs avoided, are enormous. Regulators, policy makers and individuals now face the challenge of ensuring that future generations will inherit a healthy, biodiverse natural environment, which benefits their health and wellbeing. This means both protecting people and wildlife from pollutants, and ensuring equality of access and connection to the natural environment across society.
The population of England is expected to grow by around 6 million by 2043[footnote 112], increasing the pressure on the environment caused by increased production and consumption of resources. Waste, pollution, and climate change will all create challenges in ensuring that health is not negatively affected. If habitats and biodiversity are lost, this could lessen people’s contact and connection with nature. It would also reduce many of the benefits and services provided by the natural environment. The impacts could threaten to reverse some of the health gains made over the last century. We must ensure that in creating a healthy environment in England, we do not outsource pollution and negative health outcomes to other countries through waste and emissions.
UK cities are also growing in size[footnote 113], with potential negative impacts on health and wellbeing. The design of cities to ‘accommodate, and actively encourage, a lifestyle of activity and interaction for social and physical health’ has been described by the government’s Chief Medical Officer as an urgent challenge[footnote 3]. The creation of urban green spaces will require planning so that it does not displace communities and inadvertently increase health inequalities[footnote 114].
Ultimately, human health at the species level depends on the health of the planet. How the most pressing environmental threats are managed determines human health and wellbeing now and in the future. People have an ever-increasing amount of information at their fingertips about how health is affected by the quality of the natural environment, and how they interact with it. The future health of people in England will be determined by how everyone, from governments to local communities, accesses, evaluates and acts on that collective knowledge and evidence.
References
-
World Health Organization. (1948). Constitution. Geneva: World Health Organization (Accessed 21 August 2020) ↩
-
Office for National Statistics. (2019). Measures of national wellbeing dashboard. Newport: Office for National Statistics. (Accessed 21 August 2020) ↩
-
Department of Health and Social Care. (2018). Annual Report of the Chief Medical Officer. Health 2040 - better health within reach. (Accessed 21 August 2020) ↩ ↩2 ↩3 ↩4 ↩5
-
World Health Organization. (2009). Country profiles. Geneva: World Health Organization. (Accessed 21 August 2020) ↩
-
Public Health England. (2019). News story: Public Health England publishes air pollution evidence review. (Accessed 21 August 2020) ↩
-
Public Health England. (2018). Health matters: air pollution. Guidance. London: PHE. (Accessed 21 August 2020) ↩ ↩2
-
Public Health England. (2017). Public health profiles. London: PHE. (Accessed 29 October 2019) ↩
-
Department of Health and Social Care. (2017). Annual Report of the Chief Medical Officer. Health impacts of all pollution - what do we know? Annual report of the Chief Medical officer. (Accessed 21 August 2020) ↩ ↩2 ↩3 ↩4 ↩5 ↩6
-
Royal College of Physicians. (2016). Every breath we take: the lifelong impact of air pollution. London: RCP (Accessed 21 August 2020) ↩ ↩2
-
Hussey, S. J. K and others. (2017). Air pollution alters Staphylococcus aureus and Streptococcus pneumoniae biofilms, antibiotic tolerance and colonisation. Environmental Microbiology 19:1868-1880 (Accessed 21 August 2020) ↩
-
Defra. (2020). Air Quality Expert Group: Estimation of changes in air pollution emissions, concentrations and exposure during the COVID-19 outbreak in the UK. (Accessed 21 August 2020) ↩
-
Environment Agency. (2018). State of the Environment: Air quality. (Accessed 21 August 2020) ↩ ↩2
-
Carnell, E. and others. (2019). Modelling public health improvements as a result of air pollution control policies in the UK over four decades — 1970 to 2010. Environmental Research Letters 14:74001. (Accessed 21 August 2020) ↩
-
Defra. (2019). Air pollution in the UK 2018. London: Department for Environment, Food and Rural Affairs. (Accessed 21 August 2020) ↩ ↩2
-
Air Quality Expert Group. (2018.) Air pollution from agriculture. Prepared for Defra. (Accessed 21 August 2020) ↩
-
Defra. (2017). Air pollution in the UK. ↩
-
Public Health England. (2015). Quantification of mortality and hospital admissions associated with ground-level ozone: a report by the Committee on the Medical Effects of Air Pollutants. London: PHE. (Accessed 21 August 2020) ↩
-
OECD. (2014). OECD environmental outlook to 2050: the consequences of inaction. Chapter 6: health and environment. Paris: Organisation for Economic Co-operation and Development. (Accessed 21 August 2020) ↩
-
UK Groundwater Forum. FAQs - Is the water in my tap groundwater?. (Accessed 21 August 2020) ↩
-
Environment Agency. (2018). State of the Environment: Water quality. (Accessed 21 August 2020) ↩ ↩2 ↩3
-
World Health Organization. (2017). Guidelines for drinking water quality. Chemical fact sheet. Geneva: World Health Organization. (Accessed 21 August 2020) ↩
-
Landrigan, P. J. and others. (2018). The Lancet commission on pollution and health. The Lancet 391:462-512. ↩
-
EHCA. (2019). European Chemicals Agency registrations data (Accessed 21 August 2020) ↩
-
Eurostat. (2019). Chemicals production and consumption statistics. Production of chemicals hazardous to the environment. EU-28, 2004-2017 (Accessed 21 August 2020) ↩
-
Stahl, T. and others. (2011). Toxicology of perflourinated compounds. Environmental Sciences Europe 23:38. (Accessed 21 August 2020) ↩
-
World Health Organization. (2016). Dioxins and their effects on human health. Geneva: World Health Organization. (Accessed 21 August 2020) ↩
-
Defra. (2006). Emissions of dioxins and dioxin-like polychlorinated biphenyls from domestic sources. DE0110099A. London: Department for Environment, Food and Rural Affairs. (Accessed 21 August 2020) ↩
-
World Health Organization. (2009). Biomonitoring of human milk for persistent organic pollutants (POPs). Geneva: World Health Organization. (Accessed 21 August 2020) ↩
-
UNEP. (2019). Global chemicals outlook II. Nairobi: United Nations Environment Programme (Accessed 21 August 2020) ↩
-
SAM. (2019). Environmental and health risks of microplastic pollution. Group of chief scientific advisors. Scientific opinion 6/2019. Brussels: The Scientific Advice Mechanism Unit of the European Commission. (Accessed 21 August 2020) ↩
-
Wellcome Trust. (2018). Initiatives for addressing antimicrobial resistance in the environment: Executive summary. (Accessed 21 August 2020) ↩ ↩2
-
Surette, M. and Wright, G.D. (2017). Lessons from the environmental antibiotic resistome. Annual Review of Microbiology. 71: 309-329. (Accessed 21 August 2020) ↩ ↩2
-
Ben, Y. and others. (2019). Human health risk assessment of antibiotic resistance associated with antibiotic residues in the environment: A review. Environmental Research 169: 483-493. (Accessed 21 August 2020) ↩
-
Leonard, A. F. C. (2018). Exposure to and colonisation by antibiotic-resistant E. coli in UK coastal water users: Environmental surveillance, exposure assessment, and epidemiological study (Beach Bum Survey). Environment International 114: 326-333. (Accessed 21 August 2020) ↩ ↩2
-
Mandal, J. and others. (2012). Antibiotic resistance pattern among common bacterial uropathogens with a special reference to ciprofloxacin resistant escherichia coli. Indian Journal of Medical Research 136:842-849. (Accessed 21 August 2020) ↩
-
European Medicines Agency. Undated. Antimicrobial resistance. Amsterdam: European Medicines Agency. (Accessed 21 August 2020) ↩
-
O’Neill Commission. (2014). Review on Antimicrobial Resistance: Tackling a crisis for the health and wealth of nations. Review on Antimicrobial Resistance, London. (Accessed 21 August 2020) ↩
-
HM Government. (2019). Tackling antimicrobial resistance 2019-2024: The UK’s five-year national action plan. Policy Paper. (Accessed 21 August 2020) ↩
-
DNOSES-EU. (2018). Policy Brief. Zaragoza: Distributed network for odour sensing, empowerment and sustainability. (Accessed 21 August 2020) ↩
-
Hayes, J. E. and others. (2014). The impact of malodour on communities: A review of assessment techniques. Science of the Total Environment. (Accessed 21 August 2020) ↩
-
Hänninen, O. and others. (2014). Environmental burden of disease in Europe: assessing nine risk factors in six countries. Environ Health Perspect 122:439–446 (Accessed 21 August 2020) ↩
-
Defra. (2014). National noise attitude survey 2012 (NNAS2012). Summary Report. London: Department for Environment, Food and Rural Affairs. (Accessed 21 August 2020) ↩
-
Defra. (2019). Noise action plans: large urban areas, roads and railways (2019). London: Department for Environment, Food and Rural Affairs. ↩
-
World Health Organization. (2018). Environmental noise guidelines for the European region. Geneva: World Health Organization. (Accessed 21 August 2020) ↩
-
Harding, A-H. and others. (2013). The cost of hypertension-related ill-health attributable to environmental noise. Noise and Health 15: 437-445. (Accessed 21 August 2020) ↩
-
Defra. (2010). Noise & Health – Valuing the Human Health Impacts of Environmental Noise Exposure. The Second Report of the Interdepartmental Group on Costs and Benefits noise subject group (IGCB(N). London: Department for Environment, Food and Rural Affairs. (Accessed 21 August 2020) ↩
-
MHCLG. (2014). Light pollution. Guidance. London: Ministry of Housing, Communities and Local Government. (Accessed 21 August 2020) ↩
-
Douglas, P. and others. (2017). A systematic review of the public health risks of bioaerosols from intensive farming. International Journal of Hygiene and Environmental Health 221:134-173 (Accessed 21 August 2020) ↩
-
Public Health England. (2016) Ionising radiation and you. (Accessed 21 August 2020) ↩
-
Public Health England. (2008). Ionising radiation: estimation of cancer risk at low doses. Guidance. (Accessed 21 August 2020) ↩
-
Environment Agency, FSA, Food Standards Scotland, NRW, NIEA and SEPA. (2019). Radioactivity in Food and the Environment, 2018. RIFE-24. Environment Agency, FSA, Food Standards Scotland, NRW, NIEA and SEPA: Bristol, London, Aberdeen, Cardiff, Belfast, Belfast, London and Stirling. (Accessed 21 August 2020) ↩
-
Public Health England. (2012). HPA response to the 2012 AGNIR report on the health effects from radiofrequency electromagnetic fields. London: Public Health England. (Accessed 21 August 2020) ↩
-
Lovell, R. (2018). Research Briefing: Health and the natural environment. A review of evidence, policy, practice and opportunities for the future. Defra project 14291. (Accessed 21 August 2020) ↩
-
White, M. P. and others. (2019). Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Scientific Reports 9: 7730. (Accessed 21 August 2020) ↩
-
Environment Agency. (In Press). The social benefits of blue space: a systematic review. ↩ ↩2
-
Wheeler, B. W. (2012). Does living by the coast improve health and wellbeing? Health and Place 18: 1198-1201. (Accessed 21 August 2020) ↩
-
Hillsdon, M. and others. (2011). Green space access, green space use, physical activity and overweight. Natural England Commissioned Report NECR067 ↩
-
Twohig-Bennet and Jones. (2018). The health benefits of the great outdoors: A systematic review and meta-analysis of greenspace exposure and health outcomes. Environmental research 166: 628-637. (Accessed 21 August 2020) ↩
-
Public Health England. (2017). Health matters: obesity and the food environment. London: Public Health England. (Accessed 21 August 2020) ↩
-
White, M.P and others. (2016). Recreational physical activity in natural environments and implications for health: a population based cross-sectional study in England. Prev. Med. 91, 383–388. ↩
-
Lovell, B. and others. M. (2018). Health and the Natural Environment: A Review of evidence, policy, practice and opportunities for the future. European Centre for Environment & Human Health. (Accessed 21 August 2020) ↩
-
Bell S. L. and others. (2015). Seeking everyday wellbeing: The coast as a therapeutic landscape. Social Science & Medicine 142:56-67. (Accessed 21 August 2020) ↩
-
RSPB. (2020). Recovering together: A report of public opinion on the role and importance of nature during and in our recovery from the Coronavirus crisis in England. (Accessed 28 July 2020) ↩
-
Natural England. (2020). Nature connectedness among adults and children in England (JP032). (Accessed 28 July 2020) ↩
-
Aerts, R. and others. (2018). Biodiversity and human health: Mechanisms and evidence of the positive health effects of diversity in nature and green spaces. British Medical Bulletin 127:5-22. (Accessed 21 August 2020) ↩
-
Tasnim, N. and others. (2017). Linking the gut microbial ecosystem with the environment: does gut health depend on where we live? Frontiers in Microbiology 6th October 2017. (Accessed 21 August 2020) ↩
-
Kirjavainen, P. V. and others. (2019). Farm-like indoor microbiota in non-farm homes protects children from asthma development. Nature Medicine 25: 1089–1095 ↩
-
Marmot, M. and others. (2020). Health Equity in England: The Marmot Review ten years on. (Accessed 22 July 2020) ↩
-
Office for National Statistics. (2020). Health state life expectancies by national deprivation deciles, England: 2016 to 2018. (Accessed 21 August 2020) ↩ ↩2
-
Science for Environmental Policy. (2016). Links between noise and air pollution and socioeconomic status. In-depth Report 13 produced for the European Commission, DG Environment by the Science Communication Unit, UWE, Bristol. (Accessed 21 August 2020) ↩
-
Natural England. 2009. An estimate of the value and cost effectiveness of the expanded Walking the Way to Health Initiative scheme 2009 (TIN055). ↩
-
Fecht, D. et al. (2015) Associations between air pollution and socioeconomic characteristics, ethnicity and age profile of neighbourhoods in England and the Netherlands. Environmental Pollution. 198: 201-210. ↩
-
Sheridan, C. et al. (2019). Inequalities in Exposure to Nitrogen Dioxide in Parks and Playgrounds in Greater London. Int J Environ Res Public Health. 16: 3194. ↩
-
Defra. (2018). 25 year environment plan. London: Department for Environment, Food and Rural Affairs. (Accessed 21 August 2020) ↩
-
CABE. (2010). Community green: using local spaces to tackle inequality and improve health. London: Commission for Architecture and the Built Environment. (Accessed 21 August 2020) ↩ ↩2
-
Rolls, S. (2016). Investigating the potential increase in health costs due to a decline in access to green space: an exploratory study. Research Report NERR062. York: Natural England. (Accessed 21 August 2020) ↩ ↩2
-
Natural England. (2009). Childhood and nature: a survey on changing relationships with nature across generations. York: Natural England. ↩
-
Natural England. (2019). Monitor of Engagement with the Natural Environment Children’s Report (MENE) 2018-2019. York: Natural England. (Accessed 10/10/19) ↩
-
Public Health England. (undated). Wider determinants of health tool. London: Public Health England. (Accessed 21 August 2020) ↩
-
Tunstall, S. and others. (2006). The health effects of flooding: Social research results from England and Wales. Journal of Water and Health, 4:365-380. (Accessed 21 August 2020) ↩
-
Public Health England. (2013). Floods in the WHO European region: health effects and their prevention. London: Public Health England. (accessed 21 August 2020) ↩
-
Waite, T. D. and others. (2017). The English national cohort study of flooding and health: cross-sectional analysis of mental health outcomes at year one. BMC Public Health 17:129. (Accessed 21 August 2020) ↩
-
Jermacane, D. and others. (2018). The English National Cohort Study of Flooding and Health: the change in the prevalence of psychological morbidity at year two. BMC Public Health 18: 330. (Accessed 21 August 2020) ↩
-
Munro, A. and others. (2017). Effect of evacuation and displacement on the association between flooding and mental health outcomes: a cross-sectional analysis of UK survey data. The Lancet: Planetary Health 1: e134-e141. ↩
-
Environment Agency. (2005). Flood warning for vulnerable groups. Literature review. ↩
-
Kendon, M. and others. (2019). State of the UK climate 2018. Special issue article. International Journal of climatology 39: 1–55. ↩ ↩2
-
Met Office. (2018). End of summer stats. (Accessed 21 August 2020) ↩
-
Kovats, S (eds.). (2015). Health Climate Change Impacts Summary Report Card, Living With Environmental Change. ↩
-
King, A.D. and others. (2015). Attribution of the record high Central England temperature of 2014 to anthropogenic influences. Environmental Research Letters 10: 054002 (Accessed 21 August 2020) ↩
-
Chapman, S. C. and others. (2019). Warming trends in summer heatwaves. Geophysical research letters 46:1634-1640. (Accessed 21 August 2020) ↩
-
Kendon, E. (2019). UKCP Convection-permitting model projections: Science report. Exeter: Met Office. (Accessed 21 August 2020) ↩
-
Watts, G. and Anderson, M. (eds). (2016). Water climate change impacts report card 2016 edition. Living With Environmental Change. (Accessed 21 August 2020) ↩
-
Kovats, S (eds.). (2015). Health Climate Change Impacts Summary Report Card, Living With Environmental Change. ↩ ↩2
-
Hajat, S. and others. (2014). Climate change effects on human health: Projections of temperature-related mortality for the UK during the 2020s, 2050s and 2080s. Journal of Epidemiology and Community Health, 68 :641-648. (Accessed 21 August 2020) ↩
-
Hajat, S. (2015). Health climate change impacts report card technical paper. 2. Health effects of milder winters. (Accessed 21 August 2020) ↩
-
Clayton, S. and others. (2017). Mental Health and Our Changing Climate: Impacts, Implications, and Guidance. Washington, D.C.: American Psychological Association, and ecoAmerica. (Accessed 21 August 2020) ↩ ↩2
-
Kovats, R.S., and Osborn, D., (eds). (2016). UK Climate Change Risk Assessment Evidence Report: Chapter 5, People and the built environment. Report prepared for the Adaptation Sub-Committee of the Committee on Climate Change, London. (Accessed 21 August 2020) ↩
-
Baylis, M. (2017). Potential impact of climate change on emerging vector-borne and other infections in the UK. Environmental Health 16: 112 (2017). (Accessed 21 August 2020) ↩
-
Parliamentary Office of Science and Technology. (2019). Climate change and vector-borne diseases in humans in the UK, POSTnote 597, April 2019. (Accessed 21 August 2020) ↩
-
Parliamentary Office of Science and Technology. (2019). Climate change and UK wildfire, POSTnote 603. (Accessed 29 July 2020) ↩
-
Reid, C.E. and others. (2016). Critical review of health impacts of wildfire smoke exposure. Environmental Health Perspectives 124:1334–1343. Accessed 29 July 2020 ↩
-
Environment Agency. (2019). Long-term investment scenarios (LTIS) 2019. (Accessed 21 August 2020) ↩
-
Sayers, P.B. and others. (2017). Present and future flood vulnerability, risk and disadvantage: A UK scale assessment. A report for the Joseph Rowntree Foundation published by Sayers and Partners LLP. (Accessed 21 August 2020) ↩
-
Government Office for Science. (2017). Future of the sea: Current and future impacts of sea level rise on the UK. (Accessed 21 August 2020) ↩
-
Fritze, J. C. and others. (2008). Hope, despair and transformation: Climate change and the promotion of mental health and wellbeing. International Journal of Mental Health Systems 2:13. (Accessed 21 August 2020) ↩
-
UNEP. (2020). Preventing the next pandemic: Zoonotic diseases and how to break the chain of transmission. (Accessed 28 July 2020) ↩ ↩2
-
Taylor, L.H., Latham, S.M. and Woolhouse, M.E.J. (2001). Risk factors for human disease emergence. Philosophical Transactions of the Royal Society B: Biological Sciences, 356(1411). (Accessed 28 July 2020) ↩
-
ECDC (2020) COVID-19 situation update worldwide, as of 24 July 2020. ↩
-
Office for National Statistics. (2019). National population projections: 2018-based. Newport: Office for National Statistics. (Accessed 21 August 2020) ↩
-
Office for National Statistics. (2016). Population dynamics of UK city regions since mid-2011. Newport: Office for National Statistics. (Accessed 21 August 2020) ↩
-
Hunter, R. F. and others. (2019). Environmental, health, wellbeing, social and equity effects of urban green space interventions: A meta-narrative evidence synthesis. Environment International 130: 104923. ↩

