Adult social care monthly statistics, England: February 2022
Published 10 February 2022
Applies to England
Main points
COVID-19 testing in care homes
ln the week ending 25 January 2022:
- there were around 30% fewer positive lateral flow device (LFD) tests among staff (12,059) and 25% fewer positive LFD tests among residents (1,820) than in the week ending 4 January 2022, when the number of positive LFD tests had reached its highest peak since the start of the pandemic (17,555 for staff and 2,411 for residents)
- there were nearly 70% fewer positive PCR tests among staff (10,829) and 46% fewer positive PCR tests among residents (6,854) than in the week ending 4 January 2022, when the number of positive PCR tests reached a record number since the start of the pandemic (32,760 for staff and 12,802 for residents)
- the overall number of tests conducted in care homes among staff and residents has started to decrease, after reaching record numbers in early January 2022
COVID-19 and flu vaccination in social care settings
As of week ending 25 January 2022, the proportions who had received a booster dose of the COVID-19 vaccine were:
- 88.4% of total residents and 48.9% of total staff of older adult care homes
- 78.1% of total residents of younger adult care homes
- 44.4% of total staff of younger adult care homes and 37.6% total staff of domiciliary care staff
As of week ending 25 January 2022, the proportions who had received their flu vaccination for the 2021 to 2022 season were:
- 84.0% of total residents and 25.6% of total staff of older adult care homes
- 72.7% of residents of total younger adult care homes
- 24.3% of total staff of younger adult care homes and 17.4% of total domiciliary care staff
Infection control measures in care homes
In the week ending 25 January 2022:
- 81.1% of care homes in England were able to accommodate residents receiving visitors. This has recently stabilised after a substantial decrease at the end of December 2021
- 82.7% of care homes who had staff required to self-isolate paid those staff their full wages while self-isolating. This proportion has remained consistent since mid-December 2020
- 69.9% of care homes had no staff members working in another health or social care setting. This proportion has been stable since the end of November 2021, after a period of gradual decline from April 2021
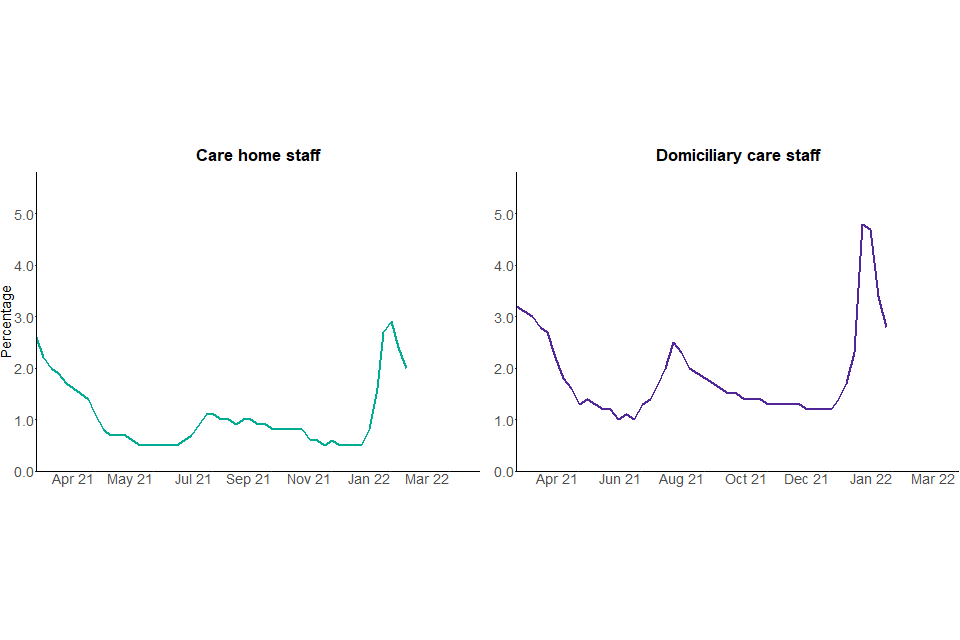
Staff absences due to COVID-19
In the week ending 25 January 2022:
- 2.0% of care homes staff were absent due to COVID-19 related reasons
- 2.8% of domiciliary care staff were absent due to COVID-19 related reasons
- absences due to COVID-19 related reasons decreased compared with the previous week, for both care homes and domiciliary care
Introduction
This is a monthly publication by the Department of Health and Social Care (DHSC) of statistics on adult social care in England. This statistical bulletin provides an overview on a range of information on social care settings, with a focus on the impact of COVID-19.
This report provides newly published information on:
-
selected infection prevention control (IPC) measures in care homes at national, regional and local authority level
-
staffing levels in care homes at national, regional and local authority level
-
staff absence rates due to COVID-19 in care home and domiciliary care at national, regional and local authority level
-
personal protective equipment (PPE) availability in care homes and domiciliary care at national, regional and local authority level
-
testing for COVID-19 in care homes at national, regional and local authority level
-
flu vaccination for the 2021 to 2022 flu season in adult social care settings at national, regional and local authority level
This report also includes previously published statistics on uptake of first, second and booster doses uptake of COVID-19 vaccinations in adult social care settings.
For more information and links to other published sources of adult social care data please see the ‘About this data’ section below.
Publication updates
Data on staff absence rates because of COVID-19 related reasons is now available. Data is available from 9 February 2021 for residential care and from 2 March 2021 for domiciliary care, and can be found in tables 5 and 6 of the accompanying ‘Infection control, PPE and workforce statistics, February 2022: data tables’.
The next publication will be published on 10 March 2022. Dates for future publications will be pre-announced on the GOV.UK publication release calendar.
COVID-19 and flu vaccination in adult social care settings
How the data can be used
This data can be used for:
-
comparing vaccination rates across local authorities and regions in England as self-reported by care providers for the:
- first, second and booster doses of the COVID-19 vaccine
- flu vaccinations for the 2021 to 2022 season
-
monitoring vaccination rates over time for the:
- first, second and booster doses of the COVID-19 vaccine
- flu vaccinations for the 2021 to 2022 season
This data cannot be used for:
- estimating the number of social care staff or residents who have not been vaccinated
- estimating the number of social care staff or residents who have been vaccinated abroad
- comparing with vaccination rates in other countries of the UK
- directly comparing vaccination take up rates between different types of care home staff (directly employed and agency staff)
- estimating the number of vaccinations delivered each day
Booster rates do not distinguish between those who are eligible for a booster, given the recommended gap between second and booster doses.
The total number of staff and residents for each social care setting as well as the number reported to be vaccinated for COVID-19 and flu are self-reported by the care provider and local authorities. As a result, the rates in this publication refer to the percentage of staff and residents reported to be vaccinated by care providers. This means that the number of individuals who have not received the vaccine cannot be directly derived from data published in these statistics as there is a number of individuals for whom the vaccination status is unknown to the care provider.
The dates in this section refer to the dates vaccinations were reported by care providers as opposed to the date vaccinations were administered.
Some care providers have reported the total number of staff or residents but not the numbers vaccinated. As a result of this, vaccination rates are affected by response rates. This is particularly prominent for vaccination rates for second doses in staff employed in other settings and boosters and flu for all staff and resident groups. This is because these groups have a lower response rate and as a result, second dose vaccination rates may be underestimated.
For data relating to 9 November 2021 and before, response rates may have been underestimated, particularly for boosters and flu vaccination. This is because the default value in the underlying data is set to zero, so any zero values submitted will appear to be non-responses. From 9 November 2021 onwards, care providers are required to select that they have reviewed their responses to confirm the data submitted is accurate, therefore increasing the accuracy of response rates.
Among care home staff, there is a substantial difference in reported vaccination rates for COVID-19 and flu vaccinations between staff directly employed by care homes and staff employed by agencies operating within care homes. This could be due to, for example but not exclusively, different uptake rates, vaccination status not being known to the care provider or the nature of employment and information available to the care homes.
For data relating to 31 August 2021 onwards, a small number of social care staff who had their vaccination outside of the UK are excluded from the numbers vaccinated.
For more information, please see the background quality and methodology note.
COVID-19 vaccinations
The NHS started administering vaccinations for COVID-19 in England on 8 December 2020. Social care staff and residents of care homes were prioritised for the vaccine according to the Joint Committee on Vaccination and Immunisation (JCVI) recommendation. For more information see Priority groups for coronavirus (COVID-19) vaccination: advice from the JCVI.
In August 2021, DHSC published operational guidance stating that, from 11 November 2021, all people working or volunteering in care homes were required to have received 2 doses of the COVID-19 vaccine as a condition of their deployment in a care home, unless exempt. More details can be found on vaccination of people working or deployed in care homes: operational guidance. However, as Omicron replaces Delta as the dominant variant, on 31 January 2022, DHSC issued a press release stating the government’s intention to revoke vaccination as a condition of deployment, subject to consultation and Parliamentary approval.
Adult social care staff and residents are still encouraged to get their COVID-19 booster vaccination after receiving their second dose. More details can be found at COVID-19 vaccination: a guide to booster vaccination.
COVID-19 vaccinations in older adult care homes
99.0% of older care homes have provided data on the number of staff and residents who received a COVID-19 booster dose, as of week ending 25 January 2022. This means the first and second dose rates, and the number of staff and residents receiving a booster dose may be underestimated compared with the true value.
For full response rates, please see the accompanying ‘COVID-19 vaccination response rates, February 2022: data tables’.
Residents of older care homes
As of week ending 25 January 2022, in older adult care homes:
- 95.9% of residents have been reported to have received 2 doses
- 88.4% of residents have been reported to have received their booster dose
Reported booster vaccination rates continued to increase across all regions throughout January, though not as steeply as seen in previous weeks. There is some variation in reported booster doses administered regionally, with the East of England region having the largest uptake with 90.4% of residents vaccinated, compared with the lowest uptake in the East Midlands with 86.5%.
Staff of older adult care homes
As of week ending 25 January 2022, in older adult care homes:
- 95.1% of staff have been reported to have received 2 doses
- 48.9% of staff have been reported to have received their booster dose
Reported booster vaccination rates continued to steeply increase across all regions throughout January. There is large regional variation in rates, with the North East region having the highest uptake with 55.4%, and London having the lowest at 39.7%.
Figure 1: percentage of staff and residents of older adult care homes who have received the first, second and booster doses of the COVID-19 vaccination, cumulative rate, 15 December 2020 to 25 January 2022, England
Reported booster vaccination rates continue to increase for both staff and residents of older adult care homes.
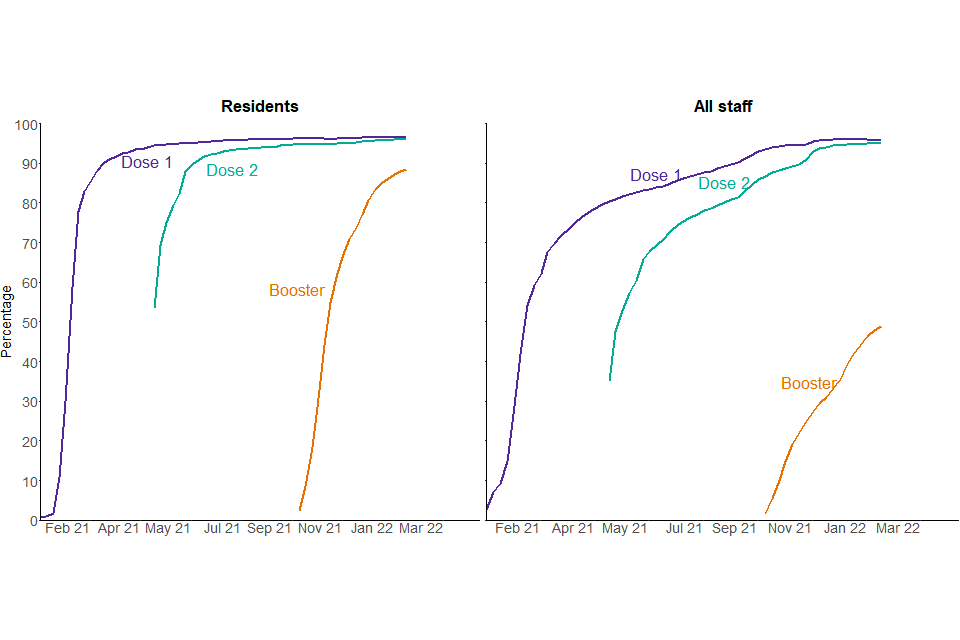
Source: Capacity Tracker
Figure 2: percentage of older adult care home staff who have received their booster dose of the COVID-19 vaccination by local authority, as of 25 January 2022, England
A majority of local authorities have a reported booster vaccination rate of between 30% and 50% for staff in older adult care homes.
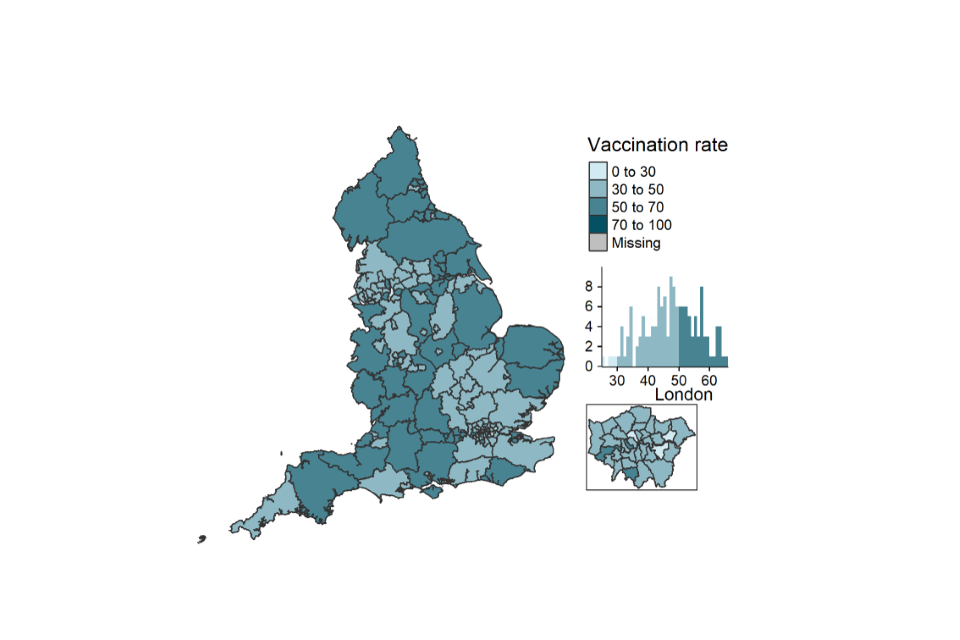
Source: Capacity Tracker
Data from figures 1 and 2 can be found in tables 1 and 2 of the accompanying ‘COVID-19 vaccination statistics, February 2022: data tables’ in addition to data by region and local authority.
Notes:
- data is reported by care providers
- data is based on date of reporting rather than date of vaccination
COVID-19 vaccinations in staff working in domiciliary care, younger adult care homes and other settings
Data for staff working in other settings (including non-registered providers and local authority employed) after August 2021 does not include Surrey as this data is no longer collected by the local authority.
The following proportions of social care staff have been reported to have received their COVID-19 vaccination doses:
In younger adult care homes as of week ending 25 January 2022:
- 93.8% of staff have been reported to have received 2 doses
- 44.4% of staff have been reported to have received their booster dose
For domiciliary care staff as of week ending 25 January 2022:
- 82.3% of staff have been reported to have received 2 doses
- 37.6% of staff have been reported to have received their booster dose
Among staff working in other settings as of week ending 25 January 2022:
- 34.6% of staff have been reported to have received 2 doses
- 4.3% of staff have been reported to have received their booster dose
As data is self-reported by care providers, COVID-19 vaccination rates are affected by response rates. An overview of response rates is in the table below.
Table 1: percentage of providers that have provided data on the number of staff vaccinated at least once as of 25 January 2022
| Dose | Younger adult care home providers on behalf of their staff | Domiciliary care providers on behalf of their staff | Local authorities on behalf of staff working in other settings |
|---|---|---|---|
| Provided data on second dose | 98.8 | 93.6 | 63.8 |
| Provided data on the booster dose | 98.2 | 90.1 | 25.7 |
Notes:
- due to these response rates, the number of staff and residents, particularly for boosters, will be underestimated compared with the true value. For full response rates please see the accompanying ‘COVID-19 vaccination response rates, February 2022: data tables’
- there is regional variation for all staff groups – please see table 2 for further details
Figure 3: percentage of staff in younger adult care homes, domiciliary care settings and other care settings who have received the first, second and booster dose of the COVID-19 vaccination, cumulative rate, 15 December 2020 to 25 January 2022, England
Reported booster vaccination rates for staff steeply increased for younger adult care home staff and domiciliary care staff.
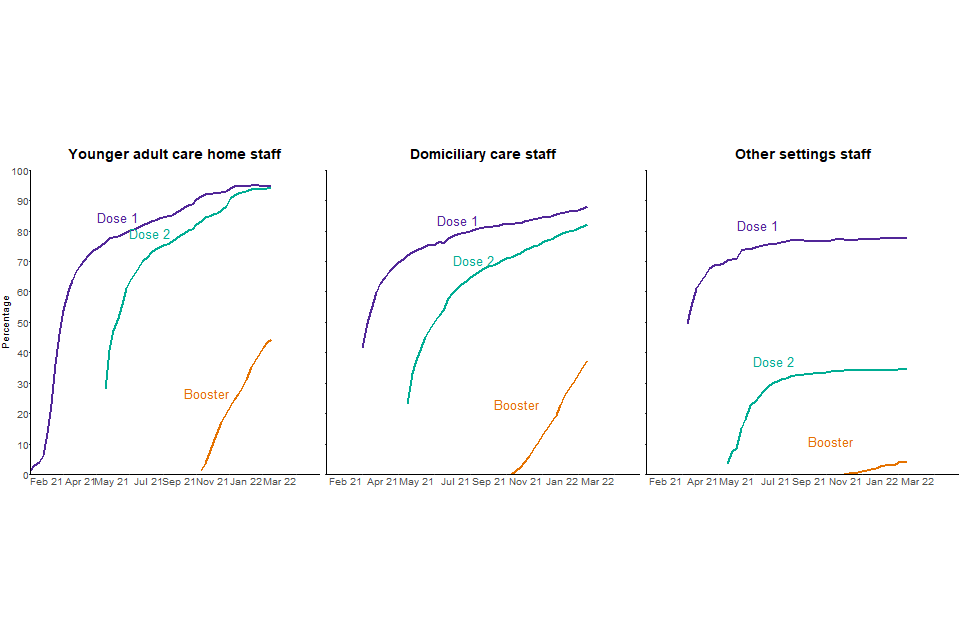
Source: Capacity Tracker
This data can be found in tables 6, 9 and 10 of the accompanying ‘COVID-19 vaccination statistics, February 2022: data tables’ in addition to data by region and local authority.
Table 2: percentage of younger adult care home and domiciliary care staff reported to have received a booster dose of the COVID-19 vaccine, up to 25 January 2022 by region, England
| Region | Younger adult care home staff | Domiciliary care staff | Staff working in other settings |
|---|---|---|---|
| East Midlands | 41.9 | 38.1 | 11.7 |
| East of England | 45.0 | 40.8 | 0.7 |
| London | 42.9 | 20.9 | 0.3 |
| North East | 59.7 | 45.0 | 8.1 |
| North West | 42.7 | 36.1 | 4.6 |
| South East | 41.7 | 42.2 | 2.6 |
| South West | 45.0 | 44.5 | 1.7 |
| West Midlands | 46.9 | 37.8 | 3.2 |
| Yorkshire and the Humber | 43.8 | 42.4 | 12.1 |
COVID-19 vaccinations for residents of younger adult care homes
Residents of younger adult care homes are not part of a single priority group for the COVID-19 vaccine. However, the conditions for which they reside in care homes are likely to make them more vulnerable to COVID-19 and they are therefore likely to be part of priority groups 3 to 9.
As of week ending 25 January 2022, in younger adult care homes:
- 92.2% of residents have been reported to have received 2 doses
- 78.1% of residents have been reported to have received their booster dose
Flu vaccination in adult social care settings
The national influenza (flu) immunisation programme aims to provide direct protection to those who are at higher risk of influenza associated morbidity and mortality. Groups eligible for NHS influenza vaccination are based on the advice of the JCVI. More details can be found in the National flu immunisation programme 2021 to 2022 letter.
This report covers cumulative flu vaccination rates for the 2021 to 2022 season in the below adult social care groups:
- residents in older adult care homes
- staff directly employed by older adult care homes
- agency staff working in older adult care homes
- staff directly employed by younger adult care homes
- agency staff working in younger adult care homes
- domiciliary care staff registered to independent CQC providers
- social care staff working in other settings (including non-registered providers and local authority employed)
- residents of younger adult care homes
Guidance on flu vaccination for social care workers was updated on 9 September 2021. For more information, please see the background quality and methodology note.
Data is self-reported by care providers and local authorities, who may submit their resident and staff numbers but not the number receiving the flu vaccination, resulting in a lower reported percentage vaccinated. An overview of response rates for the numbers vaccinated is in the table below.
Table 3: percentage of providers that have provided data on the number of staff or residents who received a flu vaccination for the 2021 to 2022 season, as of 25 January 2022
| Older adult care home providers on behalf of their staff | Younger adult care home providers on behalf of their staff | Domiciliary care providers on behalf of their staff | Local authorities on behalf of staff working in other settings | |
|---|---|---|---|---|
| Percentage who provided flu data at least once | 99.0 | 98.2 | 90.0 | 19.7 |
For full response rates please see the accompanying ‘COVID-19 vaccination response rates, February 2022: data tables’.
Older adult care homes
As of week ending 25 January 2022, the proportions of those who had received a flu vaccination in older adult care homes were:
- 84.0% of residents
- 25.6% of all staff
Younger adult care homes
As of 25 January 2022, the proportions of those who had received a flu vaccination in younger adult care homes were:
- 72.7% of residents
- 24.3% of all staff
Domiciliary care staff and staff working in other settings
As of 25 January 2022, the proportions of staff who work in domiciliary care and other settings who had received a flu vaccination were:
- 17.4% of domiciliary care staff
- 1.8% of staff working in other settings
Figure 4: percentage of social care staff and residents who have received the flu vaccination, cumulative rate, 28 September 2021 to 25 January 2022, England
The reported flu vaccination rates are highest among older adult care home residents.
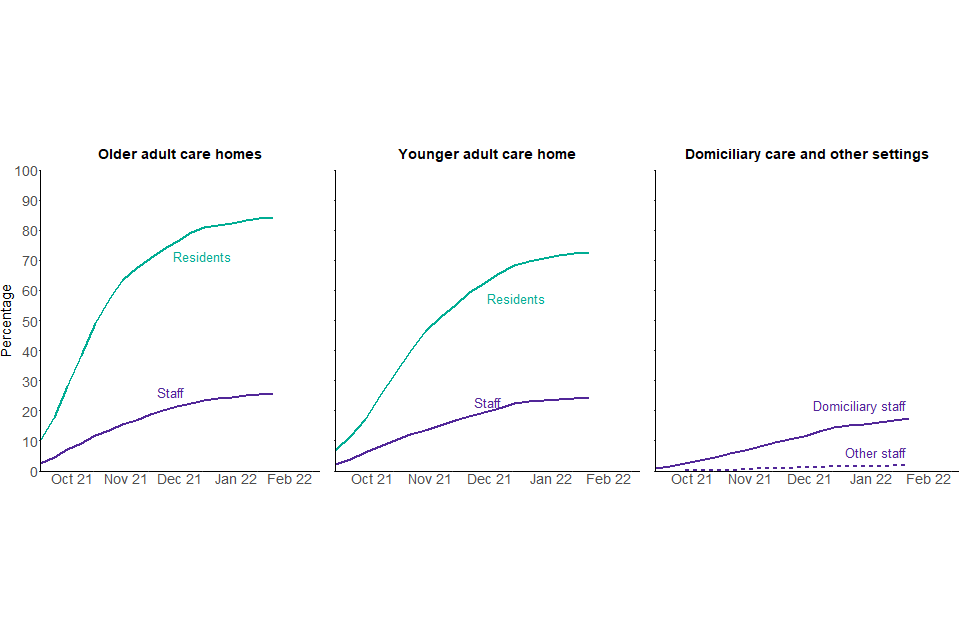
Source: Capacity Tracker
This data can be found in tables 1, 2, 5, 6, 9 and 10 of the accompanying ‘Flu vaccination statistics, February 2022: data tables’ in addition to data by region and local authority.
There is regional variation in reported flu vaccination uptake among each of the adult social care groups. The variation is most pronounced among staff and residents of younger adult care homes. Regional variation among all groups is summarised in table 4.
Table 4: percentage of each social care group reported to have received a flu vaccination up to 25 January 2022 by region, England
| Region | Older adult care home residents | Older adult care home staff | Younger adult care home staff | Younger adult care home residents | Domiciliary care staff | Other settings staff |
|---|---|---|---|---|---|---|
| East Midlands | 82.8 | 25.2 | 18.8 | 63.7 | 17.2 | 4.9 |
| East of England | 84.3 | 22.9 | 23.8 | 73.0 | 18.0 | 0.3 |
| London | 83.7 | 19.2 | 24.2 | 76.8 | 11.5 | 0.1 |
| North East | 84.5 | 27.5 | 34.9 | 77.4 | 22.3 | 3.9 |
| North West | 83.7 | 26.3 | 26.7 | 71.7 | 16.9 | 3.1 |
| South East | 84.4 | 24.7 | 23.1 | 73.4 | 19.5 | 1.3 |
| South West | 84.8 | 28.6 | 24.4 | 69.8 | 19.9 | 0.4 |
| West Midlands | 82.9 | 27.3 | 25.8 | 75.0 | 17.3 | 2.2 |
| Yorkshire and the Humber | 84.7 | 27.4 | 24.0 | 75.3 | 18.7 | 2.4 |
Infection prevention control measures
How the data can be used
This data can be used for:
- estimating the number and proportion of care homes that indicate they:
- are accommodating COVID-safe visits within the care homes in line with government guidance
- are paying full wages to the majority of their self-isolating staff
- restrict staff movement across settings
- monitoring trends over time
- comparisons across local authorities and regions in England
This data cannot be used for:
- estimating the number of visitors in care homes and their infection or vaccination status
- comparing with other countries of the UK
- linking staff movement across settings to positivity rates
The Adult Social Care Infection Control and Testing Fund provides funding from local authorities to ensure that infection prevention control (IPC) measures are in place to curb the spread of COVID-19. This publication provides data on how providers are implementing the following measures:
- limitation of staff movement across different social care settings
- accommodating COVID-19 safe visitation in care homes in line with government guidance
- payment of full wages when care home staff are isolating due to COVID-19
More details on the data collection, coverage and quality of this data can be found in the ‘About this data’ section below.
Accommodating COVID-safe visitation in care homes
The guidance on allowing care home residents to have visitors has changed since December 2020 which is summarised in the table below.
Table 5: visiting guidance since December 2020
| Date | Guidance |
|---|---|
| From 31 January 2022 | No limits on the number of named visitors, with testing and guidance to support safe visiting in place |
| From 15 December 2021 to 30 January 2022 | Residents are permitted to have 3 named visitors for regular visits with testing in place |
| 19 July 2021 to 14 December 2021 | No limits on the number of named visitors, with testing and guidance to support safe visiting in place |
| 17 May 2021 to 18 July 2021 | Residents are permitted to have 5 named visitors for regular visits with testing in place |
| 12 April 2021 to 16 May 2021 | Residents are permitted to have 2 named visitors for regular visits with testing in place |
| 8 March 2021 to 11 April 2021 | Residents are permitted to have 1 named visitor for indoor visits with testing in place |
| 6 January 2021 to 7 March 2021 | No indoor visits permitted due to the national lockdown |
| 1 December 2020 to 5 January 2021 | Indoor visits permitted with testing in place (from 19 December 2020 – no indoor visits permitted in tier 4 areas) |
Note: timelines for guidance are accurate as of 10 February 2022.
More information can be found in the guidance on care home visiting. This report covers care homes that are accommodating visitation in line with this guidance. This could cover visitation in the care homes premises, either indoors or outdoors, or also visits off premises, either for the day or overnight.
The latest relaxation of visiting restrictions came into place on 31 January 2022 and is therefore not covered by the data included in this publication, which covers the period up to 25 January 2022.
In the week ending 25 January 2022:
- 81.1% of care homes in England were able to accommodate residents receiving visitors within care homes in all circumstances. This proportion declined from 93.2% in the week ending 14 December 2021, down to 80.4% in the week ending 18 January 2022, following a change in visiting guidance on 15 December 2021. The proportion has started to stabilise in the week ending 25 January 2022
- a further 10.2% were able to accommodate visits in exceptional circumstances, which is an increase compared with 3.2% in the week ending 14 December 2021. Exceptional circumstances are individually defined by each care home but are generally thought to be considered when residents are palliative
- there is regional variation with 86.2% of care homes accommodating visitors in the South East in comparison with 75.5% in the North West
Figure 5: percentage of care homes accommodating or limiting visits for residents, 15 December 2020 to 25 January 2022, England
The proportion of care homes accommodating visiting for residents has recently stabilised after a decrease between late December 2021 and mid-January 2022.
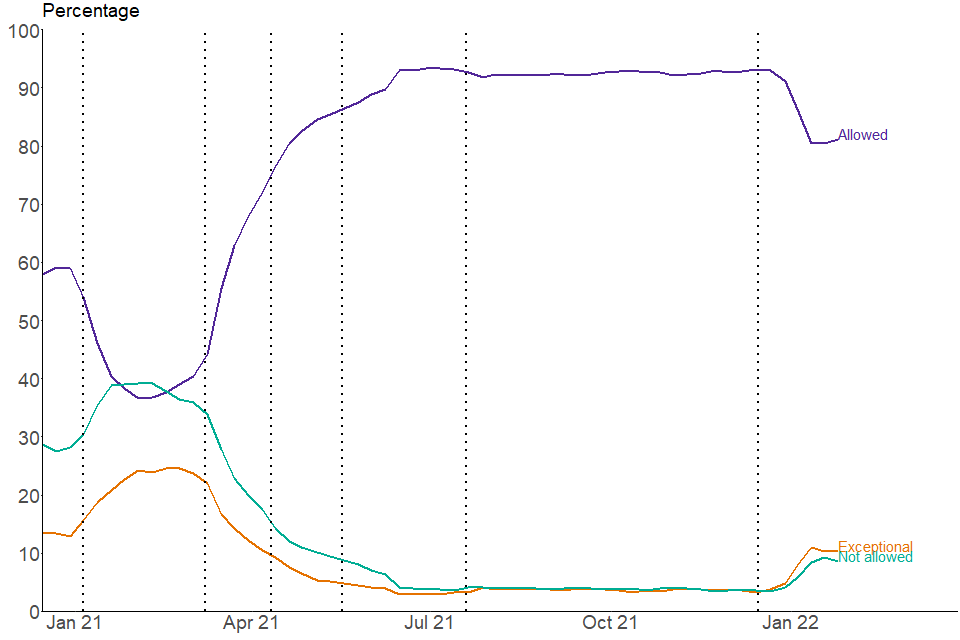
Source: Capacity Tracker
This data can be found in table 1 of the accompanying ‘Infection control, PPE and workforce statistics, February 2022: data tables’ in addition to data by region and local authority.
Payment of care home directly employed staff while self-isolating due to COVID-19
The infection control funds can be used to ensure staff who are self-isolating along with government guidance are paid their full wages. This includes:
-
staff isolating while waiting for a test
-
isolating after having tested positive or after a positive test in their household
-
staff required to quarantine prior to receiving certain NHS procedures
For more information see stay at home: guidance for households with possible or confirmed coronavirus (COVID-19) infection.
Employers who do not pay their staff their full wages while self-isolating must pay their staff at least Statutory Sick Pay (SSP) when the employee meets the following criteria:
- is classed as an employee and has done some work for their employer
- earns an average of at least £120 per week
- has been ill or is self-isolating for at least 4 days in a row (including non-working days)
Care home staff who do not meet the criteria may not be eligible and as a result not paid to self-isolate. For more information, please see guidance on Statutory Sick Pay.
The figures in this report refer to care homes which had staff required to self-isolate in the relevant week. This means care homes who had no staff needing to self-isolate will be excluded from the rates for the relevant week. There may be several care providers who may use a combination of payment options for staff wages. In these situations, providers should report the option they use for the majority of their staff.
In the week ending 25 January 2022:
- 82.7% of care homes who had directly employed staff needing to self-isolate paid staff their full wages. This proportion has remained consistent since mid-December 2020
- there is substantial regional variation with 87.4% of providers in the North East paying their staff full wages compared with 77.7% in the East Midlands
Figure 6: percentage of care homes with staff self-isolating by wages paid, week ending 25 January 2022, England
More than 8 in 10 care homes were reporting to pay their staff full wages when self-isolating.
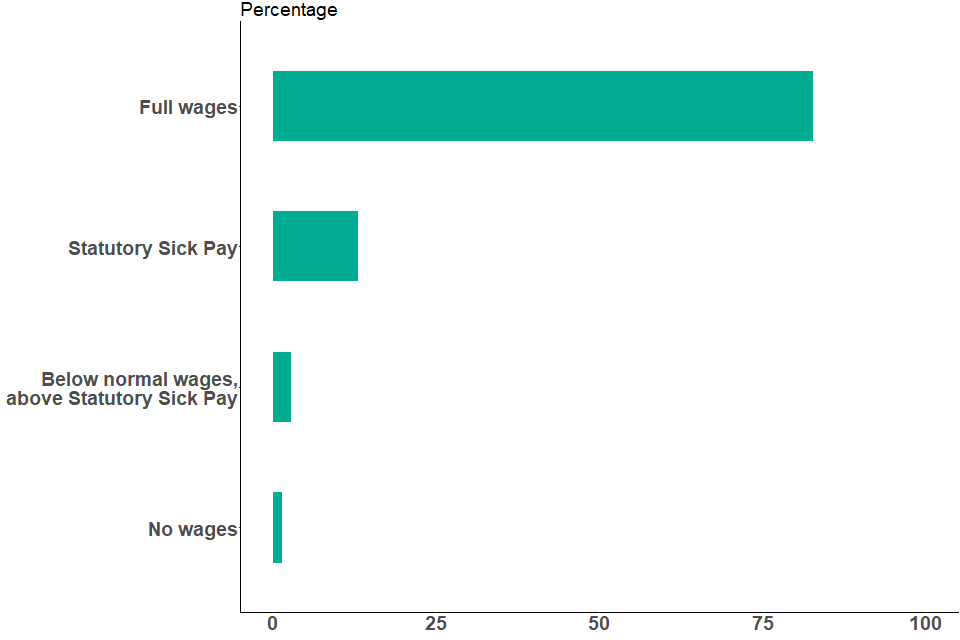
Source: Capacity Tracker
This data can be found in table 2 of the accompanying ‘Infection control, PPE and workforce statistics, February 2022: data tables’ in addition to data by region and local authority.
Limiting staff movement between care settings
Infection control funding can be used to reduce the need for staff movement between health or social care settings to limit the spread of infection, for example they can be used to recruit additional staff to enable staff to only work across one care home.
In the week ending 25 January 2022:
- 69.9% of care homes had no staff members working in another health or social care setting. This figure has remained broadly consistent since December 2021, following a period of gradual decline from April 2021
- 7.5% of care homes had some staff additionally working in another health or social care setting
- a further 22.6% of care homes had some staff additionally working in another health or social care setting due to exceptional circumstances. This number has been increasing steadily since mid-May 2021. Exceptional circumstances are defined as the care home having exhausted all other reasonable steps to ensure there are sufficient staffing levels
- there is substantial regional variation with 79.1% of providers in the North East having no staff working in another health or social care setting in the week ending 25 January 2022, in comparison with 63.8% in the South East
Figure 7: percentage of care homes by staff working across additional health or social care settings, 15 December 2020 to 25 January 2022, England
The proportion of care homes reporting having no staff working in another setting has gradually decreased since May 2021 but has remained broadly similar since December 2021.
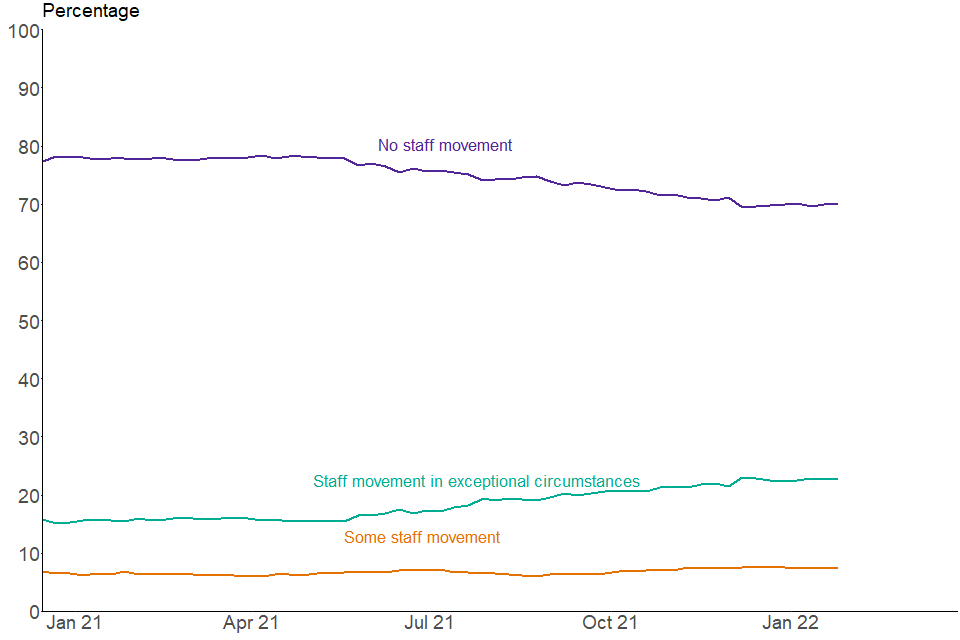
Source: Capacity Tracker
This data can be found in table 3 of the accompanying ‘Infection control, PPE and workforce statistics, February 2022: data tables’ in addition to data by region and local authority.
Care home staffing levels
How the data can be used
This data can be used for:
- estimating the number and proportion of care homes that indicate they are operating within their agreed staffing ratios
- monitoring trends over time
- comparisons across local authorities and regions in England
This data cannot be used for:
- identifying the reasons for care home staff shortages and absences
- linking staff shortages and the number of positive cases among care home staff
- comparing with other countries of the UK
In order to measure the workforce pressures on providers during the pandemic, each provider is asked to assess their workforce pressures based on their agreed staffing ratios. More details on how staffing ratios are agreed can be found within the CQC guidance on staffing.
An additional adult social care workforce report providing more information on the pressures faced by the adult social care workforce, received through an ad hoc survey, was published as part of this collection on 17 December 2021. The survey covers more detailed insight into current workforce pressures faced compared to 6 months previously. This includes issues relating to recruitment, retention, staff morale and use of agency staff.
This survey complements the regular collection by providing the opportunity to have a deeper exploration of workforce issues which is possible in an ad hoc survey but would be too burdensome for the regular collection.
Responses were collected between September and October 2021 and providers were asked to assess the pressures compared to April 2021. The key findings of the survey were:
- 70.3% of respondents reported that retaining staff was more challenging than in April 2021. 25.0% reported that it was about the same and 4.5% reported this was less challenging than April 2021
- 81.9% of respondents reported that recruiting staff was more challenging than April 2021; 15.1% reported that it was about the same; and 2.5% reported this was less challenging than April 2021
In the week ending 25 January 2022:
- 0.8% of providers flagged that their agreed staffing ratios had been breached, which is a similar level seen in January 2021. The proportion increased compared to the week ending 21 December 2021 when 0.4% of providers flagged staffing ratios being breached
- 6.6% flagged that they were operating within the agreed staffing ratios but there is a significant risk of escalation in the coming days. This proportion started to increase at the end of December 2021, reaching a peak of 6.7% in the week ending 11 January 2022
- 92.6% were operating within their agreed staffing ratios. This proportion reached its lowest point of 92.5% in the week ending 11 January 2022
If a care home’s staffing ratio has been breached, then business continuity measures may be put in place.
Figure 8: percentage of care homes operating within agreed staffing ratios, week ending 25 January 2022, England
More than 9 in 10 care homes report operating within their agreed staffing ratios.
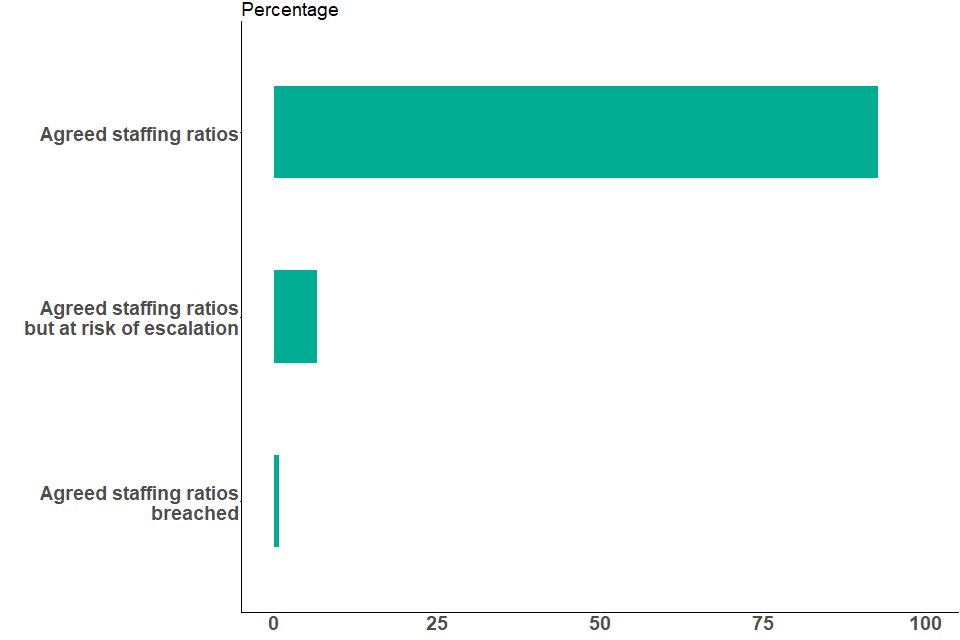
Source: Capacity Tracker
This data can be found in table 4 of the accompanying ‘Infection control, PPE and workforce statistics, February 2022: data tables’ in addition to data by region and local authority.
Staff absence rates
How the data can be used
This data can be used for:
- estimating the number and percentage of staff absent because of COVID-19 related reasons
- monitoring trends over time
- comparisons across local authorities and regions in England
This data cannot be used:
- as a sole indicator of all workforce pressures faced by the social care sector, since they only cover COVID-19 related absence.
- to directly compare absence rates related to COVID-19 between domiciliary care and care home staff
- for comparing with other countries of the UK
- for linking COVID-19 related absence rates with test positivity rates
Absence rates related to COVID-19 are calculated using the reported number of staff employed and the reported number of staff out of work that day because of COVID-19 related reasons. Both the number of total staff employed, and the number of staff absent might be affected by provider response rates as only numbers reported by providers in the last 7 days are included in the total counts.
Absence data started to be reported by care providers in Capacity Tracker from December 2020. However, low response rates in the first few months of collection mean that the workforce data is incomplete, which affects the accuracy of the absence data during that period.
Providers the least likely to respond are likely to be those experiencing the most pressures on delivery due to high levels of staff absence. For this reason, data from December 2020 to the start of February 2021 for care homes, and from December 2020 to the start of March 2021 for domiciliary care providers, are not presented in this publication.
COVID-19 related absences cannot be directly linked to staff test positivity rates. This is because absences related to COVID-19 can cover a wide range of reasons, including but not restricted to staff:
- testing positive to COVID-19
- self-isolating
- caring for someone who has tested positive to COVID-19
- suffering from illness related to COVID-19
For more information, please see the background quality and methodology note.
Absence rate statistics presented in this section have been added following a growing general interest in workforce pressures from various sources. They complement the statistics on staffing ratios presented in the previous section.
The staffing ratios statistics have not presented substantial variation over the past year, with the exception of the most recent weeks. In the adult social care workforce survey published in December 2021, however, care providers have reported facing pressures on staffing levels. This suggests that the staffing ratio statistics may not accurately illustrate these workforce pressures.
COVID-19 related absence rate statistics alone are still not sufficient to give a full picture of workforce pressures faced by the sector, however they may provide more insight on some of the challenges. Additional statistics, such as general absences, retention or recruitment could provide a more complete picture.
In care homes
Data on care home staff absences related to COVID-19 is available from 9 February 2021.
In the week ending 25 January 2022, 2.0% of care home staff were absent because of COVID-19 related reasons. Absence rates started to increase at the end of December 2021 and peaked at 2.9% in the week ending 11 January 2022, which are levels previously seen in early 2021 (see figure 9).
Variation across regions was highest in the week ending 18 January 2022 with 4.1% of staff absent because of COVID-19 related reasons in the North East, compared with 1.5% in London. In the week ending 25 January 2022, there was less regional variation, with 3.0% of staff absent because of COVID-19 related reasons in the North East, compared with 1.2% in London.
The data suggests that the size of the care home workforce has been gradually declining since April 2021. This may however be partly driven by a change in response rates over the period. A reduction in the care home workforce size is another indication of pressures faced by the sector to deliver care.
Data on workforce counts and response rates can be found in tables 5 and 10, respectively, of the accompanying ‘Infection control, PPE and workforce statistics, February 2022: data tables’ .
More information about other sources of adult social care workforce data can be found in ‘Other sources of adult social care COVID-19 data’ (in the ‘About this data’ section below).
In domiciliary care
Data on domiciliary care staff COVID-19 related absences is available from 2 March 2021. Absence rates in domiciliary care settings are not directly comparable with those in residential care homes.
Domiciliary staff COVID-19 absence rates started to increase mid-December 2021 and reached a peak of 4.8% in the week ending 4 January 2022, which is the highest level seen since the start of the timeseries in March 2021. Since then, rates have decreased rapidly to 2.8% in the week ending 25 January 2022 (see figure 9).
There has been some variation across regions, especially during periods of high absences. In the week ending 25 January 2022 regional variation has decreased compared with the previous 2 weeks, with 4.5% of domiciliary care staff absent due to COVID-19 related reasons in London, compared with 2.3% in the North West. London has consistently shown substantially higher COVID-19 related absent rates compared with other regions and reached 7.0% in the week ending 4 January 2022.
Similarly to care homes, the data suggests that the domiciliary care workforce size has been gradually declining during the last year. This may however be partly driven by a change in response rates over the period.
Data on workforce counts and response rates can be found in tables 6 and 12 of the accompanying ‘Infection control, PPE and workforce statistics, February 2022: data tables’.
More information about other sources of adult social care workforce data can be found in ‘Other sources of adult social care COVID-19 data’ (in the ‘About this data’ section below).
Figure 9: percentage of staff absent due to COVID-19 related reasons, up to week ending 25 January 2022, England
Absence due to COVID-19 related reasons has started to decrease in both care homes and domiciliary care settings in recent weeks.
Source: Capacity Tracker
Note: the proportion of staff absent due to COVID-19 reasons is not comparable across care settings.
This data can be found in tables 5 and 6 of the accompanying ‘Infection control, PPE and workforce statistics, February 2022: data tables’ in addition to data by region and local authority.
PPE availability in care settings
How the data can be used
This data can be used for:
-
estimating the number and proportion of care homes and domiciliary care providers who are experiencing PPE shortages in the next 48 hours, and comparing across local authorities and regions in England
-
monitoring trends over time
This data cannot be used for:
- predicting PPE shortages in the coming weeks
- comparing with other countries of the UK
- linking PPE shortage to positivity rates
All care homes and domiciliary care providers are responsible for ensuring safe systems of work and have duties concerning the provision and use of PPE in the workplace.
This publication covers the availability of the following 5 items of PPE:
-
aprons
-
eye protection
-
gloves
-
hand sanitiser
-
face masks
In care homes
Guidance on what PPE should be used in various circumstances is available from personal protective equipment (PPE): resource for care workers working in care homes during sustained COVID-19 transmission in England. Despite most legal restrictions being lifted progressively, PPE and other infection prevention and control measures are expected to continue to be practised in care homes.
In the week ending 25 January 2022:
- 0.2% of care homes in England had either no supply or were expecting to experience a shortage in the next 48 hours of at least one item of PPE
- this gradually decreased from late September 2020 when 1.1% of care homes were experiencing a shortage and has remained relatively unchanged since March 2021
In domiciliary care
Data on PPE availability in domiciliary care has not been updated for the London region for dates after 29 June 2021 due to a data quality issue which is being investigated. National figures for England are also not presented due to the effects of this issue on the national rate. Data for other regions and local authorities outside of London are available in the accompanying data tables.
COVID-19 testing in adult care homes
How the data can be used
This data can be used for:
- estimating the number of PCR and LFD tests taken and positive results returned in care homes, and comparing across local authorities and regions in England
- estimating trends in prevalence and positivity rates for COVID-19 in care homes based on trends in positive tests
This data cannot be used for:
- calculating positivity rates for COVID-19 in care homes due to routine and repeat testing of individuals
- linking positivity rates in care homes to lower vaccination rates in care homes
- estimating the number of people tested and positive cases in care homes as people can take more than one test
For more information on:
- the rollout of the testing programme in care homes, please see the ‘About this data’ section below.
- testing kits used, please see the ‘Terminology’ section below
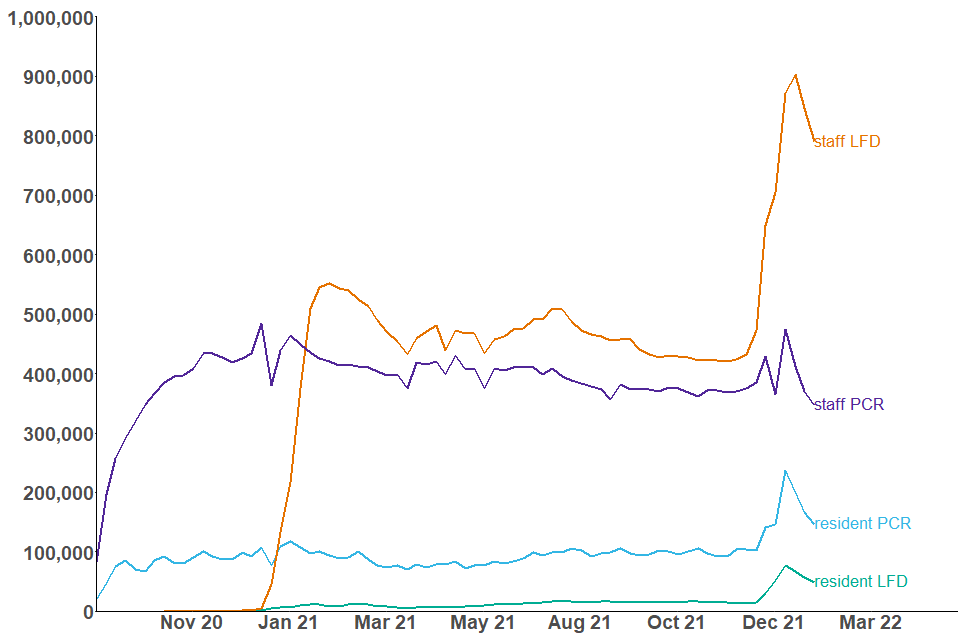
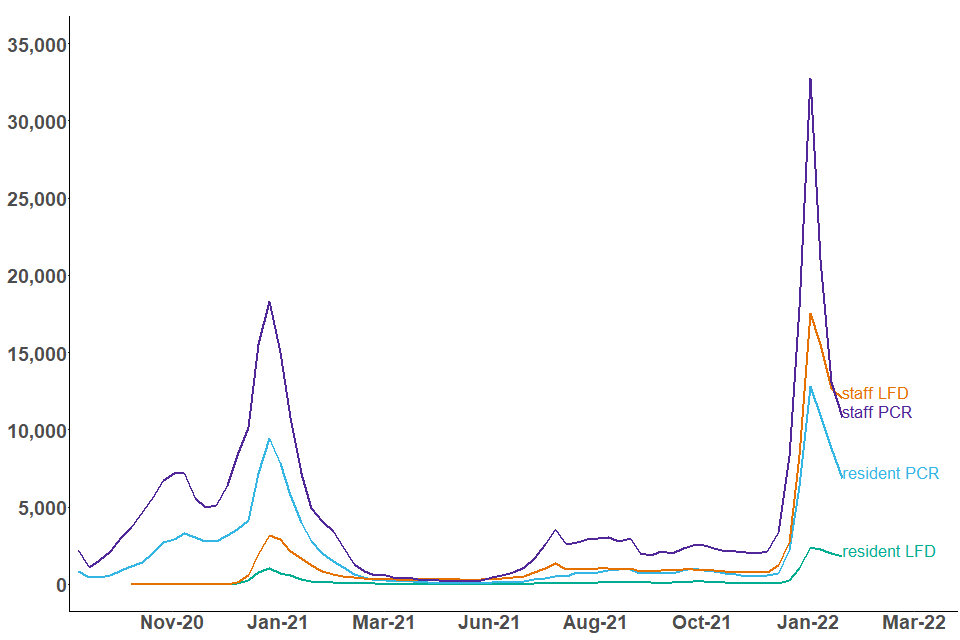
Number of tests conducted and positive tests returned in adult care homes
The number of positive tests returned in care home staff and residents increased substantially between early December 2021 and early January 2022, exceeding levels seen in summer 2021. Since the peak in the week ending 4 January 2022, the number of positive tests returned has been decreasing.
There was an overall increase in the number of tests conducted in care home staff and residents from mid-December to mid-January. This number has started to decrease throughout January 2022.
To see the latest testing regime guidance for care homes see coronavirus (COVID-19) testing in adult care homes and visiting arrangements in care homes.
Note that the guidance was updated on 15 December 2021 for staff to increase testing with LFD tests to 3 times a week, up from 2 times a week.
Guidance for the wider population, including for the care home population, also updated on 11 January 2022 to remove the need for a confirmation PCR test after a positive LFD test in most situations and to recommend the use of routine LFD testing for a period of 90 days after a positive result.
These changes are likely to have influenced the upward trend in LFD tests conducted in care homes.
Care home staff
LFD tests
In the week ending 25 January 2022, there were 12,059 positive tests returned from LFD kits in care home staff. This number decreased compared with the week ending 4 January 2022 when it reached a peak of 17,555 positive tests returned from LFD kits in care home staff, which was the highest number seen since the start of the pandemic.
The number of LFD tests conducted in care home staff, which includes positive, negative and void tests, rapidly increased between mid-December 2021 and mid-January 2022, reaching a record number of 903,409 LFD tests conducted in the week ending 11 January 2022. Since then, the number has progressively decreased down to 789,626 LFD tests conducted in the week ending 25 January 2022.
PCR tests
In the week ending 4 January 2022, the number of positive PCR tests returned in care home staff reached a record of 32,760, which is almost twice as many as the number seen in early January 2021. Since then, the number of positive tests returned from PCR kits in care home staff has decreased, reaching 10,829 in the week ending 25 January 2022.
The number of PCR tests conducted – including positive, negative and void tests – in care home staff has also started to substantially decrease since mid-January 2022, reaching the lowest level since January 2021.
The recent decrease in the overall number and number of positive PCR tests in care home staff coincides with the removal of a confirmatory PCR test after receiving a positive LFD result from 11 January 2022.
Care home residents
The testing regime for staff is more frequent than for residents. As a result, the total number of staff tests is higher than the total number of resident tests. For more information please see the ‘About this data’ section.
LFD tests
In the week ending 25 January 2022, there were 1,820 positive tests returned from LFD kits in care home residents. This number has decreased since the peak in the week ending 4 January 2022 but remains over 70% higher than the mid-January 2021 peak, when there were 1,047 positive LFD tests.
The number of LFD tests conducted in care home residents, which includes positive, negative and void tests, rapidly increased between mid-December 2021 and early January 2022, reaching a record number of 77,197 LFD tests conducted in the week ending 4 January 2022. Since then, the number has progressively decreased down to 49,464 LFD tests conducted in the week ending 25 January 2022, although the figure remains substantially higher than before December 2021.
PCR tests
In the week ending 4 January 2022 the number of positive PCR tests returned in care home residents reached a record of 12,802, which is over 30% as many the number seen mid-January 2021. Since then, the number of positive tests returned from PCR kits in care home residents has almost halved, reaching 6,854 in the week ending 25 January 2022. This recent decrease coincides with the removal of a confirmatory PCR test after receiving a positive LFD result from 11 January 2022.
The number of PCR tests conducted – including positive, negative and void tests – in care home residents has also started to substantially decrease since mid-January 2022, returning to levels seen in mid-December 2021.
Figure 10: number of tests conducted in care home staff and residents, 2 September 2020 to 25 January 2022, England
The number of tests conducted in care home staff and residents started to decrease after a peak in early January 2022.
Source: NHS Test and Trace
This data can be found in tables 1 and 2 of the accompanying ‘COVID-19 testing statistics, February 2022: data tables’ in addition to data by region and local authority.
Figure 11: number of positive test results in care home staff and residents, 2 September 2020 to 25 January 2022, England
The number of positive test results returned in care home staff and residents has decreased rapidly since the start of January.
Source: NHS Test and Trace
This data can be found in tables 1 and 2 of the accompanying ‘COVID-19 testing statistics, February 2022: data tables’ in addition to data by region and local authority.
Staff and residents have different testing regimes as outlined in the ‘About this data’ section below. As a result, the number of positive test results returned are expected to be of a different scale between staff and residents.
Visitors
The number of LFD tests conducted among visitors increased throughout December 2021, reaching 124,435 in the week ending 28 December 2021, before decreasing substantially in the first weeks of January 2022. In the week ending 25 January 2022 there were 73,813 LFD tests conducted, which was a slight increase compared to the previous week.
Additionally, there were 9,395 LFD tests conducted among visiting professionals to care homes in the week ending 25 January 2022. This is slightly higher than figures recorded since September 2021.
In the week ending 25 January 2022 there were:
- 110 positive PCR tests and 222 positive LFD tests returned in care home visitors
- 93 positive LFD tests returned among visiting professionals to care homes
Terminology
Care home: facilities providing residential care. The data in this bulletin refers to Care Quality Commission (CQC) registered care homes.
Older adult care homes: care homes serving any older people (aged 65 and over) as identified from the latest CQC data on care homes in the ‘older people service’ user band. A small number of residents within care homes serving older people may be aged under 65.
Younger adult care homes: care homes not serving any older people (aged 65 and over) as identified from the latest CQC data on care homes in the ‘older people service’ user band.
Domiciliary care: services providing personal care for people living in their own homes. The data in this bulletin refers to domiciliary staff employed by independent CQC registered providers.
Staff: unless specified, staff can refer to staff directly employed by a provider and/or through an agency.
Staff employed by other settings: this includes non-registered providers and local authority employed: all other eligible frontline social care staff working in close and personal contact with people clinically vulnerable to COVID-19 (as defined by the Joint Committee on Vaccination and Immunisation (JCVI) priority groups) who need care and support irrespective of where they work or who they are employed by, for example, local government, NHS, private sector or third sector.
Agreed staffing ratios: the agreed number of residents for any given member of staff. This is determined by individual providers to ensure there is safe levels of staffing for care to be delivered. This can be subject to inspection by the CQC. See Regulation of staffing for more information.
PCR (polymerase chain reaction) tests: PCR tests check for the genetic material of the coronavirus in the sample, which is taken using a swab and is processed in a lab via a polymerase chain reaction (PCR). These are predominantly used in care homes for people who experience symptoms, and for routine asymptomatic testing for staff and residents.
LFD (lateral flow device): often referred to as ‘rapid tests’, these test for the presence of proteins called ‘antigens’ which are produced by the virus. They are swab tests that give results in 30 minutes or less, without the need for processing in a laboratory. These tests are primarily used in care homes for routine asymptomatic testing for staff, residents and visitors.
PPE (personal protective equipment): equipment worn by staff, visitors or essential care-givers in care homes to reduce transmission of COVID-19. This publication refers to supplies of aprons, eye protection, gloves, hand sanitiser and face masks in care homes.
About this data
These statistics are being published as a part of a wider landscape of statistics on adult social care. The Government Statistical Service (GSS) compiles a UK adult social care database of official statistics on adult social care across the 4 nations of the UK. This is updated on a monthly basis.
The UK Statistics Authority (UKSA) conducted a review of adult social care statistics in England which called for:
-
better leadership and collaboration across different organisations publishing official statistics. This publication has been produced in collaboration with other statistics providers of COVID-19 adult social care data and DHSC will endeavour to work with various stakeholders as more data is published through this publication
-
addressing of gaps in available data, particularly in privately funded care. This bulletin aims to plug some of that gap by including data on residents privately funding their care in addition to those funded by local authorities
-
improving existing official statistics. These statistics are being badged as experimental statistics and more data will be added iteratively based on user needs
Other sources of adult social care COVID-19 data
COVID-19 vaccinations
NHS England and Improvement (NHSEI) also publish data on vaccinations in adult social care settings as part of their broader statistical release on COVID-19 vaccination, using the same methodology and the same data source as this publication but there are differences in the:
-
reporting period; data in this publication reports data collected up to 11:59pm on a Tuesday whereas NHSEI use data collected up to 11:59pm on a Sunday
-
a small amount of data may be collected after the respective reporting periods
-
regional breakdowns; data in this publication uses the administrative regions of England and NHSEI use NHS regions
COVID-19 testing
DHSC also publishes care home testing data in the weekly NHS Test and Trace statistics (England) at national level. This publication uses the same data source but has a different methodology for presenting testing in care homes and differences in the figures will occur due to the following reasons:
-
differences in which tests from different routes are included. Both methodologies include the number of tests registered from kits sent directly to care homes, but this publication additionally includes care home staff or residents tested via other routes such as regional or local test sites. As a result, figures in this report will be substantially higher for PCR tests conducted in care home staff due to the current guidance recommending staff with symptoms to be tested outside of the care home (see coronavirus (COVID-19) testing in adult care homes for more information). This also means that changes in the guidance for the wider population might affect the trends differently across both publications
-
different reporting periods. This publication uses the start time of the test in comparison to the Test and Trace statistics which use the date on which the test result was received by the individual taking the test
-
different times of extracting the data
For more details on the NHS Test and Trace programme and the statistics please see the NHS Test and Trace methodology document.
Adult social care workforce size and absence statistics
Skills for Care publishes yearly and monthly estimates of the number of adult social care filled posts as a measurement of the size of the adult social care workforce. Differences in data sources and methodology mean that these statistics are not comparable with those published in this report.
Skills for Care’s monthly tracking data on staffing is based on the unweighted responses of a relatively small cohort of providers who have updated records in the Adult Social Care Workforce Data Set (ASC-WDS) in each respective month. This data may not be representative of the sector as a whole and therefore may only be indicative of general trends. Skills for Care use a wider definition of ‘domiciliary care’ than is used in Capacity Tracker and include other services delivered in the user’s own home, such as supported living and extra care housing.
Skills for Care also publishes monthly estimates of the average number of days lost due to sickness, which are not comparable with the absence rates published in this report. This is because of similar reasons explained above and due to the nature of Skills for Care’s estimate which is not specific to COVID-19 related absences.
In December 2021, an additional workforce report providing more information on the pressures faced by the adult social care workforce has been published as part of this data collection. This information was received through an ad hoc survey, and has been published as part of this collection as a one-time event. Please see the adult social care workforce survey: December 2021 report.
The workforce survey complements the regular collection by providing the opportunity to have a deeper exploration of workforce issues which is possible in an ad hoc survey but would be too burdensome for the regular collection.
Data sources
COVID-19 vaccination, infection prevention control (IPC), PPE availability, absence rates and staffing levels
Data in this publication is taken from self-reported data submitted by care providers in England through a data collection and insight tool called Capacity Tracker.
Care providers are expected to submit data on IPC compliance on a weekly basis while data on vaccinations, PPE availability, staff absences and staffing levels is expected to be updated on a daily basis.
Infection control data for each reporting week refers to data up to 2pm on the date stated as the ‘week ending’ and the 7 days prior. For PPE, absence rates and staffing-levels, data relates up to 11:59pm on the date stated as the ‘week ending’. The reporting week usually ends on a Tuesday but occasionally no data is available for this date, in these situations the ‘week ending’ date will be the nearest available date.
This bulletin presents the proportion of staff and residents vaccinated out of the total number of staff and residents as self-reported by care providers. Only individuals who have not tested positive for COVID-19 in the last 28 days are eligible to receive the vaccine. Data on the number of staff and residents of older adult care homes eligible for the vaccination over time can be found in the accompanying COVID-19 vaccination tables.
For more information, please see the ‘Data Sources’ section of the accompanying background quality and methodology note.
COVID-19 testing data
Testing data is collected from management information generated during the operation of the NHS Test and Trace service.
For more information, please see the ‘Data Sources’ section of the accompanying background quality and methodology note.
Data coverage and quality
All data in this publication refers to adult social care settings in England only.
Data submitted by providers reflects the current priorities to monitor the COVID-19 pandemic in social care settings. Data collection could be subject to change based on changes to the priorities and therefore the reporting in this publication will be adapted accordingly.
IPC, PPE availability, absence rates and staffing levels
Providers are expected to submit data on IPC measures on a weekly basis while staffing levels and PPE availability data are expected to be submitted on a daily basis. Any providers who have not submitted data within the last 7 days are excluded from the relevant analysis for the associated time period where no response was received. The full response rates for all data points are available in the accompanying tables.
COVID-19 vaccinations
Data on total number of staff and residents as well as those vaccinated is self-reported by care providers and local authorities. Providers are expected to update their vaccination data on a daily basis. There may be a time lag between individuals receiving the vaccine and the week they are reported in the statistics depending on when providers have updated their vaccination data.
COVID-19 testing
This report includes the number of tests conducted on care homes residents, staff and visitors who were tested by:
-
PCR and LFD kits sent directly to the care home for regular testing, which were registered through the National Testing Programme digital infrastructure
-
PCR and LFD kits conducted at another testing site such as a regional or local test site or a mobile testing unit or tests that were registered
The figures in this report are only deduplicated to report on the number of individual tests taken, not the number of people tested. Because people can have more than one test, the data should not be compared with prevalence rates or case positivity rates.
This report does not contain data on those tested through pillar 1.
Data for each reporting period relates to the day an individual took their test.
To see the latest testing regime guidance for care homes please see coronavirus (COVID-19) testing in adult care homes and visiting arrangements in care homes.
The guidance was updated on 15 December for staff to increase testing with LFD tests to 3 times a week, up from 2 times a week. The guidance for the wider population, including for the care home population, also updated on 11 January 2022 to remove the need for a confirmation PCR test after a positive LFD test in most situations and to recommend the use of routine LFD testing for a period of 90 days after a positive result.
Any changes implemented to the testing guidance after 25 January 2022 do not impact the data included in this publication.
As of the week ending 25 January 2022, which is the latest data point included in this publication, the regular testing regime in place was as follows:
Care home staff test:
- weekly, using PCR test kits, on the same day each week
- 3 times a week using rapid lateral flow tests – one on the same day as the weekly PCR test, and an additional rapid lateral flow test every 2 to 3 days
- immediately before a shift, with a rapid lateral flow test, where they are working in multiple locations, and have worked somewhere else since their last shift in the home
- before the start of their shift on the first day back to work, after a period of leave resulting in them missing their weekly PCR, with a rapid lateral flow test (that is, after annual leave or sick leave on entry back into the care home)
- immediately if they develop symptoms, with a PCR test
Care home residents test:
- monthly, using PCR test kits
- as soon as they join a care home, if they are new, with a PCR test
- immediately if they develop symptoms, with a PCR test
Further testing may be required for visits in and out of the care home, on admission or if the resident is exposed to COVID-19.
Care home visitors:
- visitors should receive a negative lateral flow test result and report it on the day of their visit, either by conducting the test at home or when they arrive at the care home
- essential care givers will need to be supported to follow the same testing arrangements as care home staff
Visiting professionals to care homes:
- NHS professionals should provide proof of a negative test taken 72 hours in advance of the visit
- CQC inspectors regularly take weekly PCR tests but should additionally take rapid lateral flow test on the day of visiting a care home
- other professionals should be tested with a rapid lateral flow test on arrival
On 27 January 2022, a press release announced that, by 16 February 2022, care workers will be asked to use LFD tests before their shifts, replacing the current system, which included the use of weekly asymptomatic PCR tests. Care homes can transition to the new testing system anytime between the time of announcement on 27 January 2022 and 16 February 2022. The change in guidance will affect the trends in the data published in the next publication on 10 March 2022.
Different testing regimes apply when there is an outbreak of COVID-19 in a care home. See COVID-19 testing schedule for a suspected or confirmed outbreak in a care home for more details.
Revisions
Any revisions to past publications will be in line with DHSC’s revision policy and highlighted in future publications accordingly.
Feedback
For feedback and any further questions, please contact [email protected].
